This post is from an American Veteran who was given Zoloft for PTSD. The trials that brought Zoloft on the market for PTSD were negative for men. It only got a license because there were some marginal benefits in women in the trial. It has always been worrying to see troops returning from war zones being put on this and related SSRIs.
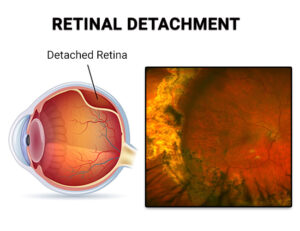
The reason for the post is to see if we can get input from anyone else put on medicine who soon afterwards developed a detached retina – or who has developed cataracts. There are suspicions that antidepressants acting on the serotonin system in particular may trigger retinal detachment and cataracts but both these eye problems and the use of these drugs are common so it is difficult to know and we need cases that are not easily explained in any other way.
Retina Detaches
On 5/11/2023 during a visit with my primary care provider at the VA, I was prescribed Zoloft for treatment of depression and PTSD. I was instructed to take one, 25mg pill once per day to help treat my symptoms.
On 3/19/2024, I was admitted to the ER for problems with my right eye. I had noticed large floaters in my eye in addition to flashes and shadows. I was seen by a doctor who said I had a torn retina and referred me to a nearby Eye Center.
On 3/20/2024, I was seen by another doctor determined that I had a horseshoe tear in my right retina in addition to a vitreous hemorrhage. He proceeded to refer me to yet another doctors who on 3/21/2024 surgically treated the eye with Cryotherapy Laser. This treatment freezes the area around the tear in the retina in order to reattach the retina to the surface of the eyeball.
On 5/12/2024, I was admitted to the ER for more problems with my right eye. I had noticed that the floaters had returned in addition to the flashes and a large shadow. I was again seen by an ER doctors who said that I most likely had a detached retina and referred me back to Eye Center the following morning. I was seen by a doctor there who validated the detached retina in my right eye. Due to surgeon availability, and need for immediate surgical care, I was referred to an Eye Specialists where I was seen on 5/13/2024.
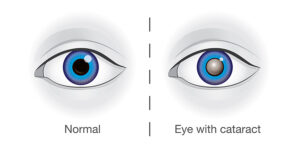
Dr. B confirmed the detached retina diagnosis and scheduled me for surgery on 5/14/2024. Additionally, she diagnosed my eyes with Lattice Degeneration which would require a recommended laser procedure to the left eye to help prevent retinal detachment there and she further stated that the right eye would develop a cataract that would require surgical treatment in order to correct it back to normal vision.
Dr. B completed the surgery on the right eye using Pars Plana Vitrectomy with Laser and C3F8 14% gas for repair of the retinal detachment. The vitrectomy procedure removes the gel-like substance that is inside the back of the eye. Gas is injected into the white of the eye (sclera), to push the eyeball back against the retina (pneumatic retinopexy). The retina was then reattached with laser treatment.
Prior to Zoloft, I had never experienced any issues with my eyes. Upon my diagnosis and during my treatment, I researched possible causes leading up to the detached retina diagnosis. I discovered that Zoloft, an SSRI antidepressant, can cause adverse ocular effects, including maculopathy, which is a pathological change in the central retina. Maculopathy can lead to reduced vision or even blindness, depending on its severity.
Some studies suggest that sertraline-related maculopathy may be caused by a number of mechanisms, including:
– Increased serotonin bioavailability which can activate phospholipase C through the 5HT2A receptor, which may increase intracellular reactive oxygen species activity and lead to retinal degeneration.
– Increased serotonin levels in the nervous system can negatively interact with photoreceptor and RPE serotonin receptors, which can disrupt the outer retinal layer and retinal pigment epithelium.
I discovered there are reports to FDA on Zoloft and retinal detachment. Although not many, these lead me to believe that my Zoloft use is more likely than not a factor in my eye decline leading up to my detached retina. I have attached the following references of scientific data and research relating to sertraline use and retinal detachment:
See Sertraline and Retinal detachment – a phase IV clinical study of FDA data, 17 Apr 2024
These eHealthme Zoloft and Sertraline posts are oddly different.
Zoloft and Retinal detachment – a phase IV clinical study of FDA data, 1 Apr 2024
Zoloft And Eye Floaters – Can Taking Zoloft Affect Your Vision?:
The image below features a cataract. Our Veteran has been told it’s likely he will need cataract surgery – that retinal detachment can make this more likely. There are reports linking SSRIs to cataract development – so it is possible there are more retinas getting detached without being noticed that we know of.
Given how many detachments there are with a lot of different drugs, in terms of making a link, it may be necessary to establish a mechanism through which SSRIs could cause problems.
These articles on PIEZO proteins and vision may offer a way forward. PIEZO proteins are in the PIEZO retina and PIEZO cornea and in their role as mechano-receptors may be playing a part in what happens in retinal and Visual Snow issues. RxISK’s first vision post – over a decade ago – Keeping an Eye on the Ball featured retinal changes.
All reports and comments welcome.

Johanna says
Just to add to the point about the paltry evidence that SSRI’s are effective in treating PTSD: A study conducted by the Veterans Administration found Zoloft to be ineffective in a military population.
https://pubmed.ncbi.nlm.nih.gov/17503980/
This is often described as a male vs. female effect, but it could just as easily reflect the wide variety of problems lumped together under the heading of “PTSD.”
Civilians being treated for PTSD are often survivors of past domestic violence or of a single traumatic event such as a violent crime or serious accident. Women diagnosed with PTSD in civilian settings may outnumber men. Symptoms of anxiety and depression may even be classified as “PTSD” based on a history of an emotionally abusive home life–and it’s undeniable that SSRI’s do make some people feel less anxious.
Combat veterans, by contrast, have often endured a 24-7 environment of extreme violence in which they were both victims/witnesses and active participants. And nothing in the treatment of civilian PTSD has explored the use of drugs to send people right back into the traumatic situations that produced the problem. Yet the military has used SSRI’s to render active-duty soldiers “fit” to return to combat — equipped with Zoloft and a rifle. The results have not been good.
annie says
December 3, 2013 271 Comments
https://rxisk.org/keeping-an-eye-on-the-ball-visual-problems-on-ssris/
Long term effects from Paroxetine –
Am I just an old person, getting older –
Waving a piece of paper in front of my eyes, I did not flinch.
The effect of numbing –
But eyesight –
Do I ascribe Paroxetine to Cataracts, Dry Eye, Macular Degeneration; paying £10,000 for implants to correct my vision.
I had a choice, go with long vision or choose to not have close vision,
Close vision is really bad, need to wear correctional vision glasses ie magnifying and pressure to go back to prescription glasses …
Was £10,000 worth it?
I’m still not sure.
Was it Paroxetine, what done my eyes in, or do those who test eyes, still don’t know the effects of SSRIs, and attribute everything to age?
All this eye surgery I had, was it really necessary, and pertinently, having had severe injuries in the past from Paroxetine, could we be on the cusp to discovering major eye damage which, unflinchingly, has a most detrimental affect on our lives …
IH says
I had perfect vision before antidepressants. As time went on, needed glasses and had astigmatism as a teen. These “meds” are highly inflammatory.
chris says
“These “meds” are highly inflammatory.”
Is that the case and if so does it link with the sensory dysregulation ?
Have been wondering about inflammation and the heat dysregulation and sensory disorder.
I also have bad close focus and need glasses for both close and long but put it down to age. You just gave me more to think about.
Dr. David Healy says
It is not clear that they are highly inflammatory – possibly the reverse – more anti-inflammatory than inflammatory. Inflammation is a huge are with many component parts – a drug could act on both inflammatory and anti-inflammatory bits of the overall pathway.
Sensory dysregulation has nothing to do with inflammation. The sensory effects begin with 30 minutes. The heat dysregulation is a real thing in its own right – almost certainly different to inflammatory effects.
The eye effects are very real and are a real part of withdrawal as well but overlooked by everyone who talks about withdrawal.
D
Louie says
In my case my vision got worse whilst taking the drug and it was progressively getting worse. Not sure how common this is. Coming off the drug resulted many new symptoms though
Louie says
That article you mention ‘keeping an eye on the ball’ was the article I read that finally offered an explanation for some unexplainable vision issues I was experiencing and after reading that I made the connection to the SSRIs.
From ages 18-21 I was getting progressively worse vision, it was getting worse very slowly and I didn’t notice it until it got to a level where I was having intense blurriness, very bad light sensitivity and this hard to explain feeling of pressure/tension from the back of my eyes that was very uncomfortable. I am farsighted and have always needed glasses for reading close up, like for reading text on my phone but this was a different kind of blurriness that was much worse than the kind you get if you don’t wear glasses, it’s like my eyes just couldn’t process what was infront of me, they felt like they were giving up as soon as I started reading a sentence and they couldn’t keep track of what I was trying to read. The light sensitivity was intense, I remember a bright summers day and I was with my friends and they were all normal and I was there shielding my eyes with my hands, squinting etc, it was not normal. And the pressure/tension feeling was absolutely vile, it’s such a hard feeling to explain but it felt like my eyes were ‘gritty’ and it’s how I’d imagine inflammation to feel like. After reading keep an eye on the ball it offered a explanation because prior to that I had been to many high street opticians and even has a comprehensive examination with an opthamologist, and nothing was ever found to be abnormal. They all said my eyes were perfectly healthy and that my glasses prescription hadn’t even changed. This is such an isolating experience because you know something is wrong but nobody knows why and I started to think that I may have some very rare neuro degenerative disease affecting my eyes that nobody could detect. I was going insane. Through the keeping an eye on the ball article I then discovered PSSD and that whole community, however it wasn’t until I came off the drug, in an attempt to alleviate the vision issues, that I started to experience the sexual dysfunction.
This is why I think ‘PSSD’ is a misnomer, it doesn’t convey the wide range of symptoms people can have, I had to discover myself that many PSSD sufferers also had visual issues. After I came off the antidepressant certain aspects of my vision improved but I still have lingering symptoms and even new occular issues like visual snow that I didn’t have prior. I also developed many new issues like bladder problems and chronic fatigue and anhedonia that were not present on the drug. So really coming off the SSRI hasn’t really been a net positive, it’s just shuffled the symptoms around a bit but the ones I’m left with are just as debilitating
Dr. David Healy says
Louie
Your description of the eye effects is quite compelling. But your eye effects are not part of PSSD. Most people with PSSD don’t have eye effects. Most people with eye effects don’t have PSSD. What both have in common is that they may start on treatment and get worse after stopping, last for decades and most people face denial of a link to treatment
D
Louie says
My sexual functioning was fine on antidepressants. I came off when I linked the ongoing visual issues to them after reading that rxisk article and saw many comments of people with similar occular issues. When I came off is when all hell broke loose, chronic fatigue, emotional numbing, anorgasmia, premature ejaculation, bladder issues etc
You can’t win with these meds, they damage you whilst you’re on them and coming off them only leads to more issues. I still have difficulties with vision, it’s very hard to explain but sometimes my eyes feel tense and I find it hard to stay focused on a single point in the distance, I’ve been told that it’s similar to what people with traumatic brain injuries get, and that’s exactly how I’d describe it – eyesight, body and mind feel like I’ve had a traumatic brain injury
I just hope for things like AI and advanced medical science to continue progressing because I feel like it’s the only way I’ll be fixed. I have so many issues, it’s going to take some kind of artificial super intelligence to untangle all this.
Harriet Vogt says
Totally recognise the clinical differentiation you’re making between the symptoms that constitute the PSSD syndrome vs the vision problems Louise is talking about.
It’s worth reflecting, perhaps, for one moment on why members of the PSSD community like Louie – and others I’ve listened to – might perceive (sic) vision problems as connected in some way to PSSD – regardless of the fact that they aren’t diagnostically. Not arguing with that.
We agree, I think, that PSSD is more than just narrow sexual deletion – it’s arguably sensual deletion. Sufferers aren’t receiving sensual signals from their bodies. In the absence of sensuality, they can’t feel.
So, it’s understandable that people like Louie – including the remarkable young woman I’ve mentioned before, (almost completely deleted by mirtazapine) who has also had debilitating vision problems that intensify when her tinnitus does – might conceptualise these DEFICITS OF THEIR SENSES as in the same zone as PSSD.
Whether the mechanisms causing all these awful harms are in any way similar is your department – I have no clue.
Dr. David Healy says
H
I agree there likely is a link between Louie’s vision and PSSD but they are still different things. When we find the answer to one it might well offer a lead in how to help the other.
We could say Louie has serotonin toxicity and leave it at that but even within the eye there are effects that he and others and likely to call Visual Blur and not Visual Snow and to get a grip on what is going on we need great descriptions of Visual Blur which at the moment ophthalmologists don’t recognise and people trying to find answers need to be aware there might to two very different conditions getting mixed together here in a way to gets in the way of pinning down what is going on and whether one or the other responds to a treatment.
D
Harriet Vogt says
D
This is *quite* a useful paper:
A Review of Ocular Complications Associated with Medications Used for Anxiety, Depression, and Stresshttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC8884704/
Especially, if you go straight to Table 2 – Common Ocular Side Effects Associated with Therapeutics Used for the Treatment and Management of Depression, Anxiety, and Stress.
SSRIs are associated with a scary raft of ocular adverse effects – but inevitably they’re listed from an ophthalmological diagnostic perspective – not patient experience. Given we do know something about the symptoms of each of these diagnoses, we can do a crude sort of mix and match, that Rxisk readers could maybe enhance. It’s difficult to differentiate one ‘blurred’ vision from another. Perhaps the experience is similar, albeit with a different cause?
These seem to be the COMMON ones associated with SSRIs:
Dry eye – light sensitive, blurry vision, itchy etc.
Mydriasis – light sensitive, blurry vision, CONSTRICTION around forehead and eyes
Intraocular pressure elevation – pain inside and around eyes, blurred vision, blind spots
Acute angle closure crisis – sudden onset severe eye pain blurred vision, halos around bright lights, nausea.
And then there are some RARE horrors: ocular dystonia, oculogyric crisis. diplopia (double vision), optic neuropathy, maculopathy.
SNRI ADEs look even more alarming including cataracts and nystagmus.
Visual snow remains a mystery.
I’ve heard and/or read you talking about dyes being the origins of ‘modern’ psychiatric drugs. I do wonder, given the extent to which their harms penetrate the human ‘fabric’, if this was such a great idea?
H
(Apologies to Louie who suffered an initial typo – Louise, oops. )
annie says
Evidence of ocular side effects of SSRIs and new warnings
https://mentalhealth.bmj.com/content/20/1/27
Do these results change your practices and why?
Yes. Ocular side effects of SSRIs are rarely recognised and have potentially serious consequences. The risk of AACG appears to be highest after initiation of SSRI treatment. At present, it is unclear whether only high-risk groups are affected by AACG, or whether this risk extends to all individuals. Regardless, the risk of AACG related to SSRIs is now the subject of updated product labelling warnings from regulatory bodies in the USA and Canada.4 ,5 Since patients are unlikely to be aware that they are at risk, prescribers should use SSRIs cautiously in those who may be more susceptible to AACG, and be vigilant if visual symptoms develop.
Monitor the eyes for ocular effects from antidepressants, anti-anxiety medications
https://www.eyeworld.org/2018/monitor-the-eyes-for-ocular-effects-from-antidepressants-anti-anxiety-medications/
Sometimes a psychotropic medication may have to be changed to help counter the ocular side effects, Dr. Riba said. Alternatively, it may be decided to stop an antidepressant or anti-anxiety agent altogether solely due to ocular side effects and switch to a different medication. The risks/benefits must be addressed, in consultation with the patient and ophthalmologist. This is especially important with chronic conditions like glaucoma, AMD, Alzheimer’s disease, and diabetes, Dr. Riba said. With the effects these conditions can have on someone’s ability to drive, live independently, and see clearly, it’s especially important to address related depression, Dr. Riba said.
‘Most effects easily managed but still require vigilance from ophthalmologists’
Way to go …
Anne-Marie says
On Mirtazapine I had very dry gritty eyes and they felt under pressure so I went and had them checked and they said I needed to be referred to an NHS optician because my pressure was above normal limits. I asked to wait for a month to see if coming off mirtazapine would make a difference and it did my eye pressure went back to normal levels.
On paroxatine I fluctuated between dilated pupil’s and constricted pupil’s. On citalopram I had constricted pupil’s.
I only noticed the dry, grittyand pressure feeling on Mirtazapine.
Dr. David Healy says
These are important observations – thanks
D
John says
I have the exact same visual issue described by another user in the comments of ‘Keeping an Eye on the Ball: Visual Problems on SSRIs’ back in 2019, which I have quoted below. I started developing it around the time I began tapering off my medication and it got way worse soon after I completely stopped them.
“It’s more than just a focus issue, it feels like my eyes are restricted, I have trouble playing computer games because I feel like I can’t see, but I can. So hard to explain, it’s harder to see things in motion and at night. There’s this weird feeling of my vision being delayed. When I shuffle through Netflix through the shows, as you sipe there’s an animation of the tiled movie titles as you pass through them. This motion makes my eyes feel like they are lagging behind trying to catch up, it’s the odd feeling like I’m drugged or drunk and it’s affecting my vision.”
Dr. David Healy says
Thanks for this – these comments are definitely food for thought. There will be 2 more vision posts coming up – they are looking for answers rather than offering answers so any further input from those commenting here would be great to get
D
tim says
Is the onset of nystagmus 3 -4 days after starting enforced fluoxetine and olanzapine (for akathisia misdiagnosed as “psychotic depression”) a visual ADR; or would this be a cranial nerve, or brain toxicity please?
Persisted after all psychotropic drugs ceased many years ago.
Thank you.
Dr. David Healy says
Tim
This is a very tricky question. I’ve turned it around in my mind several times and am not sure what option fits best. I’ve done a quick google search plus RxISK search on Nystagmus – hit the drug search option on the toolbar beside the blog option and scroll down to search by side effect. Putting nystagmus brings up a host of anticonvulsants and antidepressants.
But I would also put fluoxetine and at least one other SSRI into the drug search box and scroll down through 1000 reports for each and see what other eye problems are also listed that might possibly be nystagmus. People reporting are less likely to use the work nystagmus and ophthalmologists seem blind to any SSRI causing any adverse effects at all
Will be interested to hear what you find
D
Dr. David Healy says
Tim
I accidentally googled something that says at least one form of nystagmus is an inner ear – a vestibular – problem. Fasinating – there are very close links between vision – vestibules and proprioception
David
tim says
Thank you.
I used the RxISK Drug Search option for fluoxetine, then sertraline. Symptom Searches were reviewed using the term Nystagmus, and also Gaze Palsy.
(A Conjugate Gaze Palsy is the inability to move the eyes together in a single horizontal (most commonly) or vertical direction).
The greatest number of psychotropic drug reports were found in relation to Gaze Palsy.
Six of the first thirteen listed were as follows: Abilify. Disperdal. Sertraline. Valproic Acid. Fluoxetine. Olanzapine.
Searching under the Symptom: Nystagmus, four of the first twenty four drugs were listed: – Sertraline. Fluoxetine. Valproic Acid. Venlafaxine.
RxISK Reported, potential drug adverse reactions included: – Nystagmus. Eye Movement Disorders. (Eye Disorders).
Medical references addressing differential diagnosis all identify the importance of vestibular damage/pathology.
Drug aetiology emphasised a range of anticonvulsants (anti-epilepsy drugs) – several of which are used as
‘Mood Stabilisers’ in Psychiatric prescribing.
My concern that the rapid onset of nystagmus was either due to enforced psychotropic drug toxicity, or indicated organic brain disease (eg Brain Tumour or Multiple Sclerosis ) was treated with contempt.
Appropriate investigation was refused.
What was distressing to read during these searches were the reports of so many life-changing, multi-systems pathologies which appeared under the : – Search By Drug facility.
Many of these harms injured and maimed our loved avoidably and unnecessarily.
Abnormal Dreams. Sleep Disorder. Nocturne. Bladder/Urinary Tract Conditions. Endocrine Pathology. Temperature Dysregulation and Heat Intolerance. Tremor. Back Pain. Abdominal Pain. Abdominal Distention. Chest Pain.
Do some/all of these ADRs or chemical injuries appear on withdrawal of the causative drug, like PSSD?
Do they increase in intensity on withdrawal?
Do they appear “After the drug has left the system?
The list goes on and on thirteen years after cessation of all imposed psychotropic drugging ceased.
Our family’s experience suggests that they do.
They impair the activities of daily living, induce feelings of worthlessness and guilt.
It is heart breaking to recall the athletic, enchanting human being who lived life with boundless joy and energy before misdiagnosis, medical kidnapping, and poisoning.
We were so fortunate to have a recognised professional expert assess in detail, consult and follow the trajectory, who confirmed that there never had been any psychiatric illness or condition.
No G.P. seems able to accept this opinion, and this means that the trust needed to seek any medical help for any new illness has never been re-established.
How could any G.P. be expected to understand and endorse that the above tragedy was entirely iatrogenic.?
chris says
“No G.P. seems able to accept this opinion, and this means that the trust needed to seek any medical help for any new illness has never been re-established.
How could any G.P. be expected to understand and endorse that the above tragedy was entirely iatrogenic.?”
Your relative is lucky to have you, even my own family will not accept it let alone GP. They spy on me and report back to psych central anything that they see as unusual about my behaviour. The latest was me taking an interest in a relatives perfume being as I don’t usually ask such questions or have such interest which obviously means I could be going potty.
tim says
Disbelief, and refusal to accept that prescribed drug adverse reactions, misdiagnosed as ‘Mental Illness’ can cause such devastation to the quality of life is relentless, painful and destructive.
My wife and I are old now. Will anyone believe what really happened when we are gone?
No. Rejection and isolation are to be expected.
chris says
“Will anyone believe what really happened when we are gone?”
Well if I and everyone else on here are not gone first WE WILL !
tim says
When we re-read the series of comments above, it seemed to clarify that what we have been watching happening inexorably to our loved appears to be accelerated, premature aging caused by the cascade of enforced toxic, psychotropic drugs.
annie says
Dear Tim
It was said on the front cover of Let Them Eat Prozac
‘Controversial…Inflammatory – The Boston Globe
The Unhealthy Relationship between the Pharmaceutical Industry and Depression
David Healy
Author of The Antidepressant Era
This came out in 2004.
This was the time that some of us had just gone through monumental injurious behaviours.
I didn’t know about this book, in 2004, I didn’t know anything.
Preface
Under the Thundercloud of a Common Experience
I received a new copy of this book today, second-hand, from Amazon, at a nice-price.
I think it might do us all a lot of favours, if we go back to basics. Re-read this book and all the others I have purchased; Children of the Cure..
In this way, we get more perspective and find a better handle of where we are going.
Your daughter’s tragic outcome comes ‘Under the Thundercloud’; controversial – inflammatory; not at all.
tim says
Thank you, Chris and Annie.
chris says
Another example when people have to experience it to really grasp what is going on and it’s even worse than she has already experienced:
https://www.msn.com/en-us/health/other/my-soviet-a-e-ordeal-shows-there-s-no-compassion-left-in-the-dead-eyed-nhs/ar-BB1quRLZ
chris says
Dailymail-
“Chilling footage has emerged of a masked figure pacing outside a house that police raided after a knifeman killed two children at a Taylor Swift-themed dance workshop in Southport.”
“The person, wearing a green hoodie and a Covid-style face mask, can be seen walking back and forth outside the front door of the property around 20 minutes before Monday’s rampage, which unfolded on nearby Hart Street at around 11.50am. ”
Pacing and walking back and forth is a red flag for akathisia that few will recognise outside of here.
If the police are reading this please watch this:
Antidepressants and Mass Shootings/Murder Suicide: An interview with Dr. David Healy:
https://www.youtube.com/watch?v=CLgt3zhJ0hk
chris says
Dailymail –
“spent the entire 55 minutes of the hearing covering his whole face, with his grey sweatshirt pulled up to his hairline and at times rocking back and forth, side to side.”
“rocking back and forth, side to side”
Again a sign of akathisia
Has he been pacing in custody?
Was/is he prescribed psycotropic medication?
Connor says
Hello, I’m new to this website, but I was astonished to come across this article. I, too, experienced a retinal tear with no clear cause shortly after starting Zoloft. I had no idea there was even the slightest chance of a connection.
I’m 29 years old and I’d never had vision problems of any kind before last summer. I started taking Zoloft (25mg) again on 8/8/23 (I had previously been on it almost a decade prior while in college). Just a couple weeks later on 8/23/23 I was in the ophthalmologist’s office complaining of seeing dark floaters, and he quickly found a retinal tear and fixed it with laser surgery.
Of course, it could’ve had any number of causes— retinal tears aren’t unheard of for young people, but they’re far less common I believe. I wonder if the Zoloft could’ve been a factor. I notice that my side effects have been more pronounced and damaging this time around and I may start weaning off (I’m up to 100mg now).