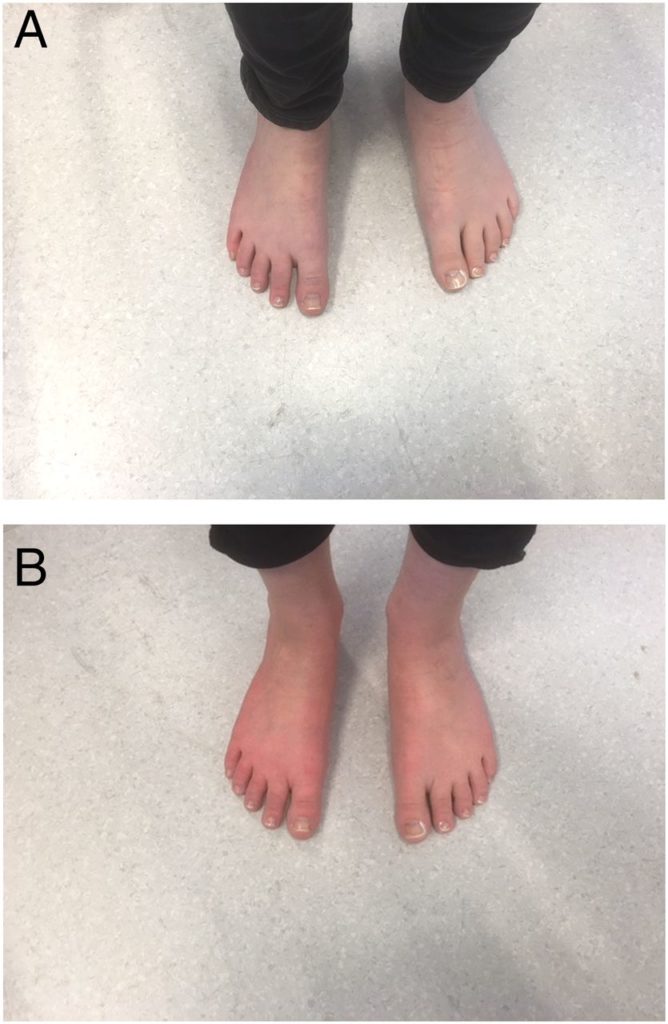
The picture here shows the before and after feet of a person who has erythromelalgia. After exercise or in response to other triggers, sometimes just lying in bed, the feet or other body parts can become hot and burning, possibly painfully so. The condition is linked to sodium channels. Those who get it may have a genetic variation predisposing them to it. Those who get it have often had an antidepressant.
Complex withdrawal
In 2015, we launched a complex withdrawal section aimed at exploring the idea that the collection of legacy effects that people often report after coming off SSRIs or SNRIs, look very similar to peripheral neuropathy – a condition in which the peripheral nerves that supply various aspects of our sense of touch stop working properly, resulting in sensory impairment and other problems.
From the start we have made close links between conditions like PSSD (post-SSRI sexual dysfunction) and complex withdrawal states. Understand one and you may well have the answer to the other. PSSD looks a best bet to research as the way in to all these problems because it is so clearly defined and its symptoms are right there on the surface of the body.
The most obvious examples of a sensory impairment from antidepressants is the genital anesthesia experienced in PSSD, or just the opposite, the sense of painful arousal that goes with PGAD.
Both PSSD and PGAD sufferers report a loss of libido, which for PSSD patients in particular is often viewed as indicating something wrong with the brain. But it makes just as much sense to view things the other way around. If the sensory input from the genitals is disturbed, this can be expected to lead to a decrease in libido.
This is even more the case when you find out that the fibers that seem most likely to be affected are C-fibers, and among the C-fiber group are a group of fibers that specifically transmit affective touch.
Many people on, or suffering withdrawal from, antidepressants report areas of skin numbness or altered sensation. These can be on the chest, back, abdomen – or sometimes the whole body. They often affect nipples, and are particularly common in feet and hands.
Sometimes people report the drug has altered the perceived pleasantness of touch sensations, such as a massage that now feels uncomfortable rather than enjoyable, or areas of the body that used to elicit a strong sexual response now feeling non-sexual or even causing a feeling of discomfort and irritation when touched.
In the complex withdrawal section we lay out the different types of nerve fibers that convey different aspects of our sense of touch. For example, some nerve fibers respond to vibrations and temperatures, while others respond to pressure. There are even specific fibers that produce a pleasant feeling when gently caressed at a certain speed – these are a specific type of C-fiber called C-tactile afferents. If something goes wrong with these fibers or the signals they process, this will give rise to unusual sensations or a change in the way we feel about being touched.
Sensory changes can have a much wider impact on our emotions and our well-being than people would ordinarily assume. For example, sense of smell is closely linked to parts of the brain involved in processing memory and emotions. Impairment of sense of smell can have a profound effect on the way we feel. Some people suffering from anosmia (loss of sense of smell) have reported feelings of isolation and emotional blunting. Smell is extremely important in the way we relate to a romantic partner.
In addition to touch, a neuropathy affecting small nerve fibers can also affect the autonomic nervous system which controls various automatic processes within the body such as heart rate, digestion, and breathing. This is called dysautonomia.
Small fiber neuropathy
A condition that has increasingly come onto our radar when thinking about withdrawal and PSSD is small fiber neuropathy.
The peripheral nerves contain large fibers Alpha and Beta, as well as small fibers such as A-delta and C-fibers. In some patients, an underlying cause such as diabetes, vitamin B deficiency, autoimmune diseases, genetic mutations, excessive alcohol intake or recreational drug use can affect the large fibers, and the same factors can sometimes affect small fibers. In others, the underlying cause can be less clear but a large variety of drugs are known to cause these problems.
In 2016, a podcast about small fiber neuropathy by Anne Louise Oaklander, Associate Professor of Neurology and director of the Massachusetts General Hospital Nerve Unit – transcript Here – laid out some of the issues.
Dr Oaklander commented that if you ask doctors to list the most common symptoms of small fiber neuropathy, they usually talk about skin numbness, tingling, or pain – often starting in the feet. However, Dr Oaklander found that when patients with the condition were asked about their symptoms, they painted a very different picture. Most of them certainly did describe altered skin sensations, but they also listed the most severe and troublesome symptoms as fatigue, tiredness, reduced endurance and strength, cognitive and memory issues, dizziness, headaches, gastrointestinal problems, bloating after meals, weight loss, diarrhea, constipation, changes in sweating patterns, and difficulty urinating.
This not only reinforces the idea that problems involving peripheral nerves can affect much more than skin sensation, but it once again describes a clinical presentation that is curiously close to the one seen in people suffering from antidepressant legacy effects, or what is sometimes called protracted withdrawal.
So, we’re asking the question – do antidepressants cause small fiber neuropathy, and is this involved in PSSD, PGAD and protracted withdrawal?
Testing
Until recently diagnosing small fiber neuropathies has not been straightforward and for this reason these conditions have remained relatively unexplored. There are currently two main tests available, but first, it’s worth explaining what type of test isn’t suitable.
When patients visit their doctor mentioning disturbances of sensation such as numbness or pain, which for over a century a doctor will link to peripheral neuropathy, they are often sent for a nerve conduction study. This involves passing electrical pulses through the arms and legs and measuring the result with a machine to assess how well the nerves are working. The problem is that these tests only investigate large nerve fibers. Patients with small fiber neuropathy typically have normal results on nerve conduction studies. The risk is you will end up being told there is nothing wrong with you – it’s all in your mind.
Quantitative sensory testing
The first type of test specifically used to assess small fiber neuropathy is quantitative sensory testing (QST). Devices which produce small vibrations and hot and cold temperatures are placed against the patient’s hand and foot, and they are asked if they can feel the sensation. The results are used to produce a graph which indicates any abnormalities in the patient’s thermal and vibratory thresholds. While this can be a useful test for detecting the presence of impaired sensation, it doesn’t specifically show that the problem is peripheral. In other words, it shows that the patient’s skin is numb, but the source of that numbness could be in the skin, the spine, the brain, or anywhere in between. Nevertheless, it’s noninvasive and can usefully show that there is indeed a problem that can be measured.
Skin biopsy
The second type of test is a skin biopsy with assessment of intra-epidermal nerve fibre density (IENFD). These tests go back a little over a decade now and have begun to come into use in many clinical settings.
A small amount of skin is extracted, generally around 3mm in diameter, one-tenth of an inch, usually from the lower leg. It is typically done under local anesthetic. The removed skin is then analysed to check for nerve fiber density.
Does this mean I have to have a skin biopsy of my penis or labia? No. In the case of both PSSD and PGAD, along with withdrawal, and also PRSD and PFS, our hunch is the damage is pretty extensive. The genital disturbance might be by far the most obvious thing but there will be in almost all cases a disturbance of sensory input to other areas too.
In the case of erythromelalgia of the feet for instance, the biopsy is taken above the ankle. With PSSD, especially if the disturbance sensations extend to inner thigh or groin as they often do, you could test there but in fact with both withdrawal and PSSD there is a good chance you could test almost anywhere.
Corneal confocal microscopy
While QST and skin biopsy are considered the standard methods for investigating small fiber neuropathy, the very latest kid on the block is another test called corneal confocal microscopy. This involves taking a scan of the patient’s eye. Its supporters claim it is more accurate than either QST or a skin biopsy. At the moment, we are not certain just what is involved or whether it is available outside of a research setting.
The paper that brought this to our attention featured the cases of two teenagers with disturbances of their feet and legs, like the erythromelalgia above. In this case the disturbances of their sensory nerves could be picked up in their eyes.
In all these cases of PSSD and withdrawal, there are likely to be fairly extensive disturbances throughout the body and these peripheral changes in many cases will explain the seemingly central changes like disturbed sleep, memory problems and loss of libido.
Help
We need anyone reading this to help us all find out where these tests can be done (ie. which hospitals or clinics) and how much they cost. You might find the tests listed under the neurology department of some hospital websites. Or you could try writing to the neurology department at your local hospital to ask if they carry out these tests, and if not, where your nearest hospital would be.
We also need PSSD and complex withdrawal sufferers to actually have QST or a skin biopsy, or ideally both, and let us know the results. If anyone manages to arrange these tests, please let us know how you did it, how it went, what it cost and what the results were.
We may be able to generate referral letters, either to a family doctor or a specialist, especially for anyone who has submitted a RxISK report on PSSD, PRSD, PFS or enduring withdrawal.
Having even a few people produce findings of abnormalities would put us in an immeasurably stronger position to raise awareness of PSSD and understand the physiology behind it.
It would also totally transform the debate about withdrawal.

Ruth says
I can relate to all these symptoms mentioned by Dr Oaklander ,
Dr Oaklander found that when patients with the condition were asked about their symptoms, they painted a very different picture. Most of them certainly did describe altered skin sensations, but they also listed the most severe and troublesome symptoms as fatigue, tiredness, reduced endurance and strength, cognitive and memory issues, dizziness, headaches, gastrointestinal problems, bloating after meals, weight loss, diarrhea, constipation, changes in sweating patterns.
I really hope this is the answer for us all.
christine says
I agree with Ruth on what Dr Oaklander found as this is all the symptoms that I have.
A neurologists answer was pills for fits.
Too scared to try this.
Spruce says
When i return to UK i will definitely try to find out if i can have these tests done. This has actually given me some real hope that i can prove that PSSD is not “all in my head”.
I will probably need a supporting letter from Rxisk, as nearly all the doctors at my doctors surgery are sceptical about PSSD.
There is one doctor who was semi believing about PSSD, and i feel he might be persuaded to refer me to a neurologist. I definitely want to get tested and will do everything i can on my return to get referred.
Also i wanted to mention i really think Rxisk are definitely onto something in saying that PSSD is caused by a small fiber neuropathy. It makes a lot of sense to me; even more so after reading this article.
Whenever i get the small improvements in my PSSD it seems to be to do with something with the nerves in my genital area, especially around the testicles. I get a feeling like the nerves are trying to re connect, but are only slightly “touching”. This has happened consistently time and time again. I am almost convinced now that PSSD is more to do with the nerves than the brain etc.
I have waited so long for some real leads and answers to PSSD. I have waited 10 years. I am very hopeful that this small fiber neuropathy theory for PSSD will turn out to be correct.
Please do not give up Rxisk team. I really think you are on the right tracks. Also if protracted withdrawal can also be officially acknowledged from this, then that is even better still, as most doctors dont believe withdrawal symptoms can last longer than a few months at most.
The sooner we can get PSSD and protracted withdrawal officially acknowledge, the better. Then people wont have to go through the isolation and misery of dealing with PSSD and enduring withdrawal all on their own, because it will be acknowledged as real.
Spruce says
Also of note.
Whenever my genital numbness is at its worst (it fluctuates regularly from being very bad where my genitals almost ache with numbness, to being milder), both my scalp and feet feel a bit numb (but not to the same extent as my genitals).
This lesser but noticeable numbness in my scalp and feet only is noticeable when the genital numbness is really bad. I dont know if this is helpful in mentioning.
susanne says
Is there any connection with restless legs syndrome? – the inner restlessness and burning sensation and redness of the skin is similar I have seen it in a relative and it’s very distressing.
Dr. David Healy says
S
You haven’t been reading all the blogs. There totally is a link – especially obvious with PGAD, which looks in many respects like a form of akathisia.
Either that or you have been reading all and we just haven’t make it clear enough. Watch out for a post soon
D
mary H. says
Since we suspect that there are very many sufferers and certainly doctors, who, possibly, do not read the Rxisk blog posts, might it be an idea to have a letter that we could print out and take to our local doctors surgeries/ CMH centres asking if they know of centres where these tests can be done? The more centres found, the better I guess.
Also, is there any point in those who are not suffering from PSSD, but regularly list the other symptoms mentioned, making enquiries about these tests? I’m thinking, in particular, of the sensations of feeling uncomfortably cold when no one else feels even cool, which is suddenly replaced by feelings of being ‘on fire’ whilst remaining within the same room with no change of temperature. (Maybe that reaction is already understood and named of course, in which case I will understand that it falls outside of this category).
With reference to the loss of sense of smell and/or taste – the only time that mine work effectively is if I have to be on steroids for my asthma. It is only then that I realise what I’m missing. My pleasure in eating, generally, has to be by the different textures; pleasure of nature simply by the different hues never the scents.
For the last week I have been living on low carb. and, magically, I’m beginning to taste food – only slightly, but certainly a marked difference. I doubt whether any of this is of relevance – but, if nothing else, it does show how tiny changes can sometimes make an unexpected difference.
Dr. David Healy says
The odds are that most complex withdrawal problems, including from drugs like quetiapine involve a degree of Short Fibre Neuropathy. We have been trying from the start to keep people with both akathisia on the one hand and withdrawal on the other hand on board. PSSD and PGAD seem a very clear example of what happens in akathisia and complex withdrawal
D
chai says
dr healy, do you find a deferent neurobiological damage of pssd made from ssri and anti psychotics like risperdal ?
do you find a connection betwin pssd, pois (post orgasmic illness syndrome) and chronic fatigue syndrome ?
i got them all together at age 13 from risperdal.
Dr. David Healy says
Risperdal and ssris give a different sexual damage I think. POIS is a different condition again. Not sure re links to CFS
D
tim says
Please may we have a little more detail re
Risperdal / SSRIs cause a different sexual damage?
This exploration and debate around small fibre neuropathy is fascinating. There may be implications for such a wide range of medical specialities, and so many patients.
I perceive that the prevalence of SFN in those multiply injured by psychiatric dugs may be very high?
Painful hands (intermittent) and colour changes analogous to erythromelalgia feet illustrated above cause daily distress in our experience.
Dr. Oaklander’s podcast transcript made compelling reading.
Laurie O says
Mary, low carb makes a world of difference for me as well. If I have more than 10% carbs, or more than about 35 g in a day, there is hell to pay when trying to get to sleep. Mostly temperature fluctuations and anxiety. Slight restless leg. It’s like a predictable cycle I just have to get through and takes about 2 hours. These particular problems came on gradually after I finally got off Seroquel. I didn’t have this in Klonopin withdrawal and I’ve attributed it partly to menopause. Not a cure all and not easy at times but I’ve been doing keto for about 8 months and have noticed some cognitive improvements as well.
Johanna says
Casting around for news of the corneal confocal microscopy (CCM) test, I kept running into one group of researchers over and over — at the Univ. of Manchester. (It did seem to be in use in the USA, but almost exclusively in eye diseases per se. Especially those that might be treated by expensive and highly speculative stem-cell therapies. That’s where the big money is, I guess.)
But in Manchester they’re excited about its use in diabetic neuropathy, a less profitable but much more widespread problem. CCM seems to correlate well with small-fiber damage both in the hands & feet, and in hard-to-study places like the heart and other internal organs. It could be used to diagnose such damage early. Or evaluate which treatments might slow it down over the long run. They have also used it to study folks with a neurological disorder called Charcot-Marie-Tooth (CMT) which involves both large- and small-fiber damage. The role of the small-fiber damage has always been more mysterious.
The lead author on most of these studies was a Prof. Rayaz Malik who studies endocrinology and diabetes at the U of Manchester. However, a couple of people on his crew also work out of the Salford NHS Trust. They seem like the kind of people to whom sheer intellectual curiosity is not entirely alien. If they could not do this test on PSSD sufferers themselves, they might be glad to help you figure out where in the UK to get it done.
mary H. says
Johanna, I think the Manchester Uni. work is also linked with Liverpool Uni. Have been in touch with my niece who is a medical statistician/ researcher there asking if she is aware of any of this. (I seem to recall that her team did something about diabetes at some point therefore worth a try anyway).
Hs h says
Do you also have ideas in treating this. There was a paper wrtten by waldinger where they used low power laser irradiation therapy
Dr. David Healy says
We have mentioned this in posts and on the website. The hope behind the RxISK Prize is to get someone building on what has already been done to come up with a way to make a bid difference
D
Meschelle says
I had the skin biopsy test for small fiber neuropathy done by Dr. Chemali at Sentra Hospital in Virginia Beach, VA. I have PSSD but this test was done for dysautonomia and it was covered by my insurance so I don’t know what it would’ve cost otherwise. My results were normal. They also do this testing at Johns Hopkins in Baltimore, MD.
Terry hall says
Any research or new ways of identifying this would be most welcome , we need new treatments and fast I’m 4 years into horrendous withdrawels with all the above symptoms and showing no signs of healing and still to this day I am told by my doctor that’s it is all in my head ,
gv says
did you do a biopsy?
Ketiperri says
Dear Healy, what do you think it will the cure for drugs caused progressive toxic enchephalopathy too???? I mean when everyone had got severe adverse reaction on 1month use med with severe cognitive and emotional symptoms and it is only worsen 2and half year later? Thank you
Dr. David Healy says
I think they are probably linked
D
Karl says
David do you think severe ssri withdrawal could be a kind off encephalitis I have wondered this before ?
Dr. David Healy says
i kind of neuritis rather than encephalitis I think
D
Karl says
Thankyou David The pains I had in my head for years constant aren’t as bad now but I have had symptoms in all parts off my body but the constant head pressure pain was the worse like somthing out a horror film couldn’t believe what was happening to me and it went on for years no let up like a constant torture. I still get brain zaps when drifting to sleep some nights but not as often and have had periods off months where the zaps disappear then reappear. I feel the effects off these drugs affect all bodily systems like you have said before. I feel like I suffered some kind off traumatic brain injury nervous system damage never been the same but not as bad as the start. Recently told I have fibromyalgia but I’m sure this is related to what happened to me wake up in the morning feel like I’ve been run over by a truck I have huge long term memory problems since I stopped but short term memory is okay.
Christian Forbear says
Ketiperri. I was diagnosed with Lexaoro induced Toxic Encephelopathy. Are you in my Neurotoxicity Facebook Group. It’s for people that are not necessarily in withdrawal. But had toxic reactions to SSRIs. Like the people that have committed suicide. The difference is we are still alive fighting a battle that we can’t seem to win. Look for us and me too if you like.
Karl says
How was you treated for it ? I am interested on what symptoms you had could you provide a link to your Facebook group story ?
Antonia Schachter says
Please provide a link to the group as there are many! Thanks 🙏🏻
Marksanchez says
If this theory is right this could be the answer:
https://www.sciencedaily.com/releases/2017/11/171108155538.htm
Heather R says
This reference is very interesting – mentioning ‘chemotherapy induced nerve damage’. As the acne drug (Ro)Accutane isotretinoin was also developed as a chemotherapy drug, ((this being the prescribed med, several courses of which led to our son’s akathisia and then suicide), and as so many of those taking it get PRSD; if the PRSD is indeed nerve damage, then maybe we can now see why. And hopefully, now do something to restore normal working order. Psychotropic prescribed meds for the RoAccutane-induced never-ending ‘low mood’, added to the PRSD caused by them as well, plus a mini psychosis from the synergistic effect of the two kinds of medication.
Heather R says
Another thing, maybe totally irrelevant, but in my son’s paternal family Raynaud’s disease is common. My husband has it quite badly, his feet when he gets out of bed in the morning look exactly like the picture of the red swollen feet in DH’s post. One toe never ‘feels’ any more, at any time, and sometimes turns blue black in colour. He has reported all this to the GP who ran blood vessel conduction tests and they were ok. Whilst driving, his fingers go white and feel numb, they lose all sensation. His own father and brother had/have this too. So maybe our son had an inherited gene tendency already for nerve damage and RoAccutane could have accentuated it?
susanne says
There are 2 Consultants Neuro-opthalmologists listed for the Birmingham and Midlands Eye Centre. Lydia Alverez and Timothy Mathews. Referrals welcome from all areas of UK. Need referral letter from GPs to include :
Sub speciality requested, Referral details – name of GP, practice name/address. phone no. date of referral – Patient details – name, sex, d.o.b. NHS/rxk No. address/phone no. Medical history, Current meds, Significant history, including previous consultants seen, Active problems, clinical info. Request routine or urgent? Reason for referral, Preliminary investigations including management appropriate to reason for referral, Also info regarding special/social circumstance Does person have mentalhealth or mobility difficulties, interpreter needed?
Some of the above could be tricky depending how the referral letter is written I would want to see a copy myself.
Another option in the Birmingham are is – BMI The Priory Hospital tel. 01214402323 Consultant neuro-opthalmologist Mike Burdon. A private first consultation is between £150 – £250. They would accept referrals from any health professional not necessarily just a person’s GP.
Spruce says
Meschelle; wouldn’t it be disappointing if everyone with PSSD got tested for small fibre neuropathy, and they all came back with normal results.
Dr. David Healy says
Not necessarily. If there is an abnormality on biopsy etc, this points to damage which while it may not be permanent is not helpful. Its possible to have a peripheral neuropathy with a disturbance of function rather than a loss of nerve fibres.
If the biopsies and CCN are all normal, the next step is to explore gene testing for sodium and other ion channel genes. These may or may not be somewhat more reversible
David
Meschelle says
I wasn’t able to get tested until 2016 – three years after Lexapro withdrawal and beginning of my PSSD. I wonder if I had some structural neuropathy that had healed to the point of being undetectable by the biopsy test (although my PSSD did NOT heal) but left functional damage. I’d be interested in genetic testing.
Katie B-T says
I see my optomologist in early May and I’ll ask him about the corneal confocal microscopy. My hunch is that the skin biopsy may pick up the small fiber neuropathy in some areas of damage but not others. I think it will be clearer to know where to take the sample for the feet vs the bladder or autonomic nerves. My experience w nerve blocks for the pelvis also makes me think that where exactly the sample is taken will make a difference. However, I could be totally wrong.
How far along is the science for sodium and calcium genes that may be relevant to our purposes? I don’t know anything about genetic testing.
Carla says
Frozen feet at night and hot feet during the day.
I don’t know which one is worse.
I’m staying away from those pesky tests that don’t conclude anything.
Not all tests conclude a solid diagnosis.
Why would I want to subject myself to further harm?
There must be an infra red scan, of some kind, that determines thermal temperature through out ones body.
I’m done with being a lab rat.
I was a pin cushion, when I had a very bad adverse reaction and no one cared to tell me what I was going through when I was being maltreated.
What would more tests conclude and what would more meds do?
Sorry to sound pessimistic but I would rather put up with all the medical issues I have than be subjected to tests, jabs and meds ~ that’s me!
mary H. says
Isn’t it wonderful to see everybody pooling their efforts and moving ahead with this? Spruce, I can understand your tension about it – hence your thought of what if all tests came back normal but I’m sure that, deep down, you can see that ALL avenues have to be attempted otherwise nothing can possibly be gained. I appreciate that, because you want a cure so much, you dare not even set your mind on that possibility incase of further disappointment. Maybe now, more than ever, is the time for all of us to be thinking very positive thoughts and be grateful that, at last, things seem to be on the move. Good luck to all who go ahead and have a test done – I shall look forward to hearing about them. We must remember that without going ahead and being tested we will grind to a halt again; that would be such a disappointment for us all I feel.
Spruce says
Of course I will go ahead and get tested Mary H, and I am trying to stay positive.
This small fibre neuropathy theory has offered the best hope yet in my opinion, of finding a real way forward with PSSD.
I was just pointing out how disappointing it would be if the testing didn’t really lead to any solution etc.
I was feeling a bit pessimistic about things the day I made the comment.
Johanna says
Re: the link sent by Mark Sanchez: Here’s the underlying research paper, and the researcher heading this up, Anne Louise Oaklander MD. Right now her team is testing intravenous immunoglobulin (IVIg) in people with painful peripheral neuropathy that is “apparently auto-immune.”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5791555/
http://www.massgeneral.org/doctors/doctor.aspx?id=17253
They have also estimated up to 40% of people “labeled with fibromyalgia” may have a condition of this sort. Since one popular theory of fibromyalgia is that it is “really depression,” and since it’s been so widely treated with Lyrica and Cymbalta even by doctors who don’t subscribe to that theory, I wonder if some of those 40% are suffering from an effect of their treatment?
I have to admit being leery of some of this … We’re talking about treatment with powerful immune-modulators which can cause pretty drastic effects, and are ruinously expensive (and thus wildly profitable). When I clicked on the Science Daily article my screen lit up with ads for Enbrel and Rituxan. And some of the splashy publicity coming out of Mass General/Harvard — that both Fibro and Irritable Bowel Syndrome sufferers may now have “HOPE,” or that a new class of “non-narcotic pain relievers” will solve our opioid problems — hints that someone is angling for an ENORMOUS market of people for whom the treatment may be far worse than the disease. (Search Pub Med for the works of AL Oaklander and you will find — hurrah! — they are all free for download alla sudden.)
Still, they may be on to something important–especially if a limited course of therapy rather than long-term treatment could solve some of these problems. Wouldn’t it be ironic if a lab at one end of Mass General identified some of the damage being done by the enterprising Psychiatric Vanguard at the other end of Mass General? Watch your back, Doctor Oak!
Carla says
Many health issues are NOT GENETIC.
They are drug (prescribed medicines) induced.
Until, there is transparency, accountability and all concerned taking responsibility for the HARM these meds have caused, sadly we are always going to hear the same nonsense, over and over again.
Dr. David Healy says
Carla
Tuberculosis is genetic. More so that for instance schizophrenia. It is highly heritable. This means that if you have a certain genetic make-up you are more likely to catch it. It doesn’t mean genes cause it. Even if you have these genes, the tubercle germ causes tuberculosis.
In the same way, only some of get bad withdrawal or akathisia from SSRIs. Doesn’t mean these genes cause it. The drug does. Finding if there is genes and if you have these genes doesn’t mean they’ve caused it. They help prove you have what you say you have
D
Carla says
David,
Not all tests are black and white. There are many shades of grey.
When many of us needed support and answers, in our times of need, they (they know who they are?), left us in a lurch.
Many of us know, what we suffer with and unless we are seeking compensation, many of us do not have to prove anything to anyone.
If one understands how western medicine works, it is not what it all seems to be.
Western Medicine is a big scam.
Western medicine creates many of the problems and then they want a pat on the back when they find a cure for what they induce.
This is not healing it is about business and money.
Dr. David Healy says
C
Non-Western medicine is an even bigger scam. Anywhere people are vulnerable there will be rip off merchants. The biggest problems in the Western medicine case are a set of lies – one that we let companies get by claiming they have the science on their side when we aren’t let see the data. The second is that doctors make a comfortable living out of drugs being available on prescription only – this is done to protect us – but they aren’t living up to their side of the bargain. Aside from that …
D
Carla says
David,
I completely agree with you.
Sadly, when we have a medical problem (s), we rely on so many people in the healing profession to be our saviour.
Some people swear by them, whilst others believe it’s all hocus pocus.
What other choices do the vulnerable have?
Carla says
Interesting to note that lupus also affects the central nervous system.
https://www.hopkinslupus.org/lupus-info/lupus-affects-body/lupus-nervous-system/
Ruth says
One of my worst and most enduring symptom is a balance problem it is a constant rocking and feeling of motion when I am still. I have noticed that my feet don’t feel connected to the floor and wonder if this is neuropathy?
Carla says
How many brain injuries are a result of prescribed medications?
And how many brain injuries are misdiagnosed and mislabelled?
– encephalitis
– cerebritis
– vasculitis of the blood vessels of the brain
– ischemic stroke
– cranial neuropathy
and any other brain damage that these prescribed medicines induce.
What worries me, is if it is misdiagnosed and labelled as dementia, a mental disorder or some other incorrect diagnosis.
Brain injuries do result from prescribed medication.
I should know because I have a permanent problem that resulted from an adverse drug reaction.
Seventeen years later, it is still there and I know what I have to deal with however, I keep it to myself.
If I had had all the unnecessary tests back then, I most likely would not be here today.
So, yes, it pays to be stubborn, sometimes.
Hence, the reason why I preserve myself the best way I can.
The damage is done and further tests, in my opinion, just adds to further humiliation and more problems.
Mike says
For what’s it’s worth, I had an EMG test done on my legs and hands and they found sensory neuropathy in my feet (not my hands-although both remain numb). They didn’t check the genital region. They tried to play it off as mild in my feet, but if these medications caused large fiber neuropathy in my feet, imagine what they did to other parts of the body! Even more scary is what has been done to my brain neurons? MRI scans of the prudential nerve was clean. Although I’m not sure an image of that nerve would provide any indication of malfunction in that nerve. The PFS guys with severe ED are said to have severe neuropathy of the prudential nerve. Dr. Healy, any idea what test they are using to find that neuropathy? Would an EMG show more of a functional dysfunction of a nerve rather than just a visual inspection?
Dr. David Healy says
Thanks for this. Very helpful to get. You are right – if there is large fiber neuropathy there is likely to be small fiber neuropathy also. We need to get as many people as can to take as many different tests as they can and see if we can discern a pattern in the findings.
David
Petr says
I´m suffering from PSSD. I have been doing some literature research looking for polyneuropathy and its causes, especially toxic polyneuropathy. I´m quite sure there is connection especially in regard to C-fibres. My symptoms consist, apart from the whole cascade of PSSD, from numbness of scalp, particular insensitivity to touch – I would say I can identify topographic position of the touch, basic qualities, but any emotional retine is missing – my body is not able to recognize sensual touch, carring, caressing etc. Just plain neutral touch. It is annoying. It has many consequences: I don´t feel my children cuddling with me, my partner trying to engender erotic touch and atmosphere, I don´t feel peeple if they hug me. I´m isolated, cutt off my body, cut off any pleasure my body was used to convey before SSRI. I have also particular anosmia, again I can smell something but completely without any affective respond. Fine and subtreshold scent are undetectable not triggering any reaction . My erotogenic areas ceased to generate any thrill and pleasure, the same is with kissing – I used to love kising my partner – nowdays it conveys nothing – sometimes felt even disgusting – it triggers no thrill. Another interesting symptom I suffer from is sensation of permanent lack of light – like dimmed vision – it is peculiar and as expected nothing wrong with my eyes on standard ophtalmotologist assesment. I gave myself trial with B vitamins with no avail. There is much more to report. What will be the best place to report, David?
Dr. David Healy says
Petr
This is a wonderful description. One of the best I have read. If you can send a more detailed one to david.healy@rxisk.org, it might work well as a post in its own right but also as a good description to send to researchers we are in touch with to help trigger their interest.
David
susanne says
David -Can we be told which researchers are interested? Are they near to agreeing to do research?
Dr. David Healy says
Suzanne
The main group we have been liaising with are in Maastricht but no one at present is near to doing anything. Its never easy to approach a research group who are busy researching their ideas with an idea that is not one of theirs.
The key thing to nail down is whether there is gross nerve damage – c fibres probably – that can be detected on skin biopsy or CCM – if not then the right group for us will be one that deals in the genetics of sodium or other channels which would cause nerves to malfunction rather than be missing – hence the need for people to get tested – and to continue to provide good descriptions of the problem that might help some research group make a connnection.
D
chai says
dr healy, i made my small fiber biopsy a week ago so i dont have the resolts yet.
i did QST of the penis and BCT and they were normal.
ill do MRN for the pudendal nerve and MRI for my spine this month too.
i allready new that my tectile sensation was normal but its the sexual sensation, libido and unhedonic orgasm that are destroyed.
what medical test would be best to do now ?
is the fact that my pssd is a resolt of risperdal and not ssri requires deferent tests ?
Sally Macgregor says
Are C fibres involved in tardive distonia/dyskinesia? Tried googling but nothing comes up. I’m not sure if anyone knows what causes TD except it’s been linked to messing around with dopamine by antipsychotics (and dopamine agonists in Parkinsons). And affects muscle function. Hope I haven’t missed this somewhere.
PCNG says
What the hell are they doing to us?
http://www.dailymail.co.uk/news/article-5621297/Painkillers-sent-gay-says-man-broken-girlfriend.html
Anonymous says
I had QST done previously at San Diego Sexual Medicine when first looking for help with PSSD. Abnormalities were detected. Here is the doctor’s write-up:
Quantitative sensory testing used the right pulp index finger as the control site. The test sites were the glans penis, right lateral shaft and left lateral shaft penis. Vibration perception threshold values were 4 volts, 5 volts, 4 volts and 4 volts, respectively. The cold perception threshold values were 21 degrees, 12 degrees, 16 degrees and 12 degrees, respectively. The heat perception threshold values were 30 degrees, 40 degrees, 39 degrees and 39 degrees, respectively. Quantitative sensory testing reveals elevated vibratory, cold and heat perception threshold values. Results of this test are abnormal and are consistent with mild-moderate sensory neuropathy of the dorsal nerve branches of the pudendal nerve.
Anonymous says
Hi, same person back with more test results. I was able to get a Corneal Confocal Microscopy done by Penn Ophthalmology. Unlike the QST, the results of the CCM looked normal.
Dr. David Healy says
Thanks for this. Good to know
D
Altostrata says
Interesting that the withdrawal symptom of burning might be related to sodium channels. Would taking potassium counter this, I wonder?
I am going to suggest this to people experiencing the burning sensation and conduct a bit of an observational field study (see our discussions about burning http://tinyurl.com/yd6ybtta
http://tinyurl.com/y93oqtqe
http://tinyurl.com/y7tl65t2
As people experiencing psychiatric drug withdrawal syndrome are often hypersensitive to internal stimuli as well as external (and drugs in normal doses as well), a very small lowering of the intensity of the signal might not trigger the hypersensitivity reaction.
On SurvivingAntidepressant.org, we also frequently see a withdrawal symptom people describe as “restless leg” that often responds well to magnesium supplementation (glycinate or citrate), magnesium oil, or Epsom salts baths (magnesium sulfate). As magnesium counters calcium, I wonder if the calcium channel is involved, causing abnormal muscle tension, again in the context of hypersensitivity.
Dr. David Healy says
Alto
Thanks for these suggestions. They map onto details we lay out on our complex withdrawal page where we run through what is known about TRP channels on which Magnesium etc works.
We don’t seem to be able to get people to go to this page and begin to engage with the issues. This is an area that needs crowd-research. I’m not in a position, or even want to be in a position, to direct people to try this or that based on what is known about TRP channels but I do wish people would investigate this more and hope that some investigating might involve some testing safe options out and reporting back as to whether there are any effects – good or bac
The one thing rxisk has taught me is that the average person has a great capacity to research these things and get good answers – motivation is worth more than expertise in my view. The expert input we can get from reporting back to others and this can help keep feet on the ground but waiting for an expert to find answers is a mug’s game
David
Ravi says
Is there a clear magnesium/calcium ratio that can be measured? I had very high Calcium on my blood tests
Ravi says
Would this theory be able to account for people getting windows of improvement? I frequently see people reporting 50% improvements in symptoms before returning to baseline. Surely small fibre neuropathy would necessitate our symptoms staying relatively constant?
Also if it does turn out to be the main issue, will there eventually be a feasible path to recovery?
Dr. David Healy says
Ravi
One of the features of small fibre neuropathy is it can show windows of improvement
DH
Ruth says
Are there any theories as to why some people suffer enduring problems for years while others don’t. Surely any damage to nerves or cells would affect everyone?
christine says
This is a really good article on the trp receptors, just need someone now to find the tests that we need.
The G Protein–Coupled Receptor–Transient Receptor Potential …
pharmrev.aspetjournals.org/content/67/1/36
Sensory nerves are equipped with receptors and ion channels that allow them to detect and respond to diverse chemical, mechanical, and thermal stimuli. These sensory
Expendable says
This idea again seems interesting, but I do not believe that there is real nerve damage here. There have been too many resolved cases, and too many cases with windows (even my own massively improved window w/ Licorice Root) for me to believe it. It’s in the right ballpark, but not in the right glove, y’know? Perhaps it’d be worth looking into a different mechanism for the same symptoms, like the ion channel business.
Ryan says
I have had PSSD for four or five years now. In the beginning I was convinced that PSSD was a brain disorder of some sort; a hormonal imbalance, chemical imbalance, damage to neurons, or the serotonin system etc. When I read Healy’s idea a couple years ago PSSD was likely a peripheral issue, or an issue in the peripheral nervous system, I thought it was ridiculous. I wouldn’t even consider it. Yet, the more time that goes by, the more I am starting to think we should take that possibility seriously based on my experiences. The depression and emotional issues that I had a the beginning of PSSD have for the most part resolved. It is now primarily the sexual aspects that remain. The sexual aspects have remained consistent and unchanged over five years, even while the emotional issues and depressions issues have lessened. I do think this is further confirmation that PSSD is not just caused by depression BTW. As the other issues have lifted, it feels more and more like a physical issue. If our condition was the result of major changes in the brain, doesn’t it seem likely that further changes in the brain leading to less depression, and or greater capacity for emotion would in turn lead to SOME changes in my sexual condition? Yet it has not. I have less sensitivity in my genitals, and much less ability to feel pleasure through them just as did when I first got PSSD. I have a reduced response to itching and touching certain parts of my body; almost as though there is a disconnect from my conscious experience to the sensation. I also have no sex drive. I think it is possible that somehow the communication between the genitals and the brain is what is damaged, and many sexual feelings, even feelings of sexual attraction and sexual desire, not just physical pleasure, may in fact rely on a complex communication between the genitals and the brain.
Any neuroscientist will tell you, there is no one “sex” region in the brain, so it has always been a mystery to me as to how we could lose some or most of our sexuality given the de-centralized nature of sexuality in the brain. Damage to, or changes within, one section of the brain is unlikely to explain our condition. Doesn’t it make more sense that the communication between the genitals and the brain is required for the experiences of sexuality, and that damaging this communication system could greatly reduce or eliminate our sexuality? LESS SENSITIVITY IN THE GENITALS IS PERHAPS THE MOST COMMON SHARED SYMPTOM of PSSD, doesn’t that seem like a peripheral issue, and not a brain issue?
This possibility does not of course eliminate the possibility that damage to the communication system also causes changes in the brain, such as hormonal balances BTW. It is not therefore necessarily inconsistent with the fact that PSSD and PFS sufferers experience changes in hormones and neurosteriods. Perhaps those changes are more EFFECT than CAUSE.
Zeipii says
Any theory on how the windows work in the nerves/brain? I have lost the ‘feeling’ of my stomach as well as appetite as a part of my pssd. Somehow this loss of feeling of the stomach and also feeling of deep breath is gone, together with loss of skin sensitivity on scalp, arms, back and genitals. Also suffering total anhedonia, and thinking all this somehow goes together and is caused by damage of some sort at least in the brain but maybe also nerves. I also have tickling of my feet.
Zeipii says
…. and is there any knowledge of if such neuropathic damage can heal over time? This I mainly relate to my question about the windows (I never had any in 14 mths unfortunately). If such problems can have windows, what causes them and can the same phenomenon eventually cause healing?
Linus says
Dear RxISK Team,
I’d like to give a brief overview about my complex withdrawal sufferer story to support your research acitivties.
I took Maprotiline at dosis of 10 mg per day for about 30 years to address psychosomatic disorders. I experienced the typical side effects as weakness and tiredness, dry mouth,
skin more sensitive to sunlight than usual, changes in appetite and weight, blurred vision, changes in sex drive or ability, see https://medlineplus.gov
Liver enzymes alanine aminotransferase and glutamate dehydrogenase increased.
In 2015, I was diagnosed with glaucoma.
In 2014, I got the recommendation to replace Maprotiline by Citalopram and Escitalopram. I had to stop treatment with Citalopram and Escitalopram after a couple of months as I experienced migraine aura every second day.
From May till October 2015 I took Mirtazapine, phased in at 15 mg, increased up to 45 mg per day. and phased out in 6 weeks interval 45 mg, 30 mg, 15 mg, 7,5 mg.
I have experienced all kinds symptoms linked to protracted syndromes, especially
Increased anxiety
Restlessness
Muscle tightness and stiffness and twitching
Food and drug sensitivities or intolerance
Fatigue
Taste or smell changes
Sensitivity to sound and light
Visual disturbances => visual snow syndrome
Auditory disturbances => tinitus
Memory and concentration problems – Brain Fog – Chemo Brain
Brain zaps
In 2015 I noticed the first symptoms of a small fiber polyneuropathy with burning, tingling, and prickling (paresthesia) feet. Step by step the symptoms extended to the hands and mouth (burning mouth syndrome)
The diagnosis idiopathic small fiber polyneuropathy is based on a skin biopsy performed in August 2017, see below, extensive blood analysis and gentests.
Skin biopsy:
Findings:
In the skin of the lower leg with normal thickness of the epidermis, the number of intraepidermal nerve fibers is reduced to 3.2 fibers per mm, the subepidermal nerve plexus reduced, sweat glands are not presented.
In the skin of the thigh, with normal thickness of the epidermis, the number of intraepidermal nerve fibers is 7.7 fibers per mm normal, the subepidermal nerve plexus is reduced, sweat glands are not presented.
Assessment: Reduced distal and promixal intraepidermal nerve fibers without evidence of significant inflammation.
Best regards,
Linus
L says
“Measurement of electrochemical conductance of penile skin using Sudoscan®: A new tool to assess neurogenic impotence.” 2017
https://www.ncbi.nlm.nih.gov/pubmed/28528745
Sudoscan: an innovative device for early detection and follow-up of Autonomic and Small Fiber Neuropathy.
Deb says
I was on Zoloft and switched to lexapro 3 tines in 3 week period. Body freaked out and quit after 3 weeks. Full body tingling , insomnia, vibrating then turned to full body neuropathy. Diagnosed with autonomic small fiber nuropathy 50% degeneration by biopsy. I have no emotions, full body numbness and tingling. Muscle atrophy, subcutaneous fat loss, face abs skin atrophy. Living a hell the past 2 months. Can’t poop regular, feel intimacy. Teeth even shifting. Feels like I have brain damage. Forgot to do similar things. Help I’m in hell!!!!
Lily says
I was on Prozac for about 9 months. 6 months after going off of it I got really really sick. It started with allergies. I have no idea if the Prozac was a factor or not but after being super sick and losing 40 lbs over the last year, I have tested positive for SFN and every day is a living nightmare. I know I am going thru hormonal stuff too but I can relate to the last poster about whole body tingling, numbness and no emotions. I also have so many other symptoms, too many to name. It is so scare to think this could be my life indefinitely. It is hell.
GV says
How are you now Deb?
Tim says
I am late to finding this article, though I’ve been familiar with Dr. Healy’s hypothesis that PSSD is at least in part the result of some peripheral neuropathy. In addition to all the standard symptoms, my PSSD symptoms, which I’ve had for almost 15 years now, include an ambient cold burning sensation in my legs, stretching down to my feet. I can sometimes feel this burning in my genitals, as well. The burning is most prominent when sitting. I almost discount this because it often seemed like I was the only one who experienced it, but now I’m starting to think I should highlight it whenever I see a doctor (though I have mostly given up trying to get help from them).
It seems others have felt burning in addition to the standard numbness and lack of response to touch as well. Have others felt this cold burning in their legs? As I type, it’s very prominent, and it’s not a pleasant sensation, though not painful.
It seems very much like peripheral neuropathy to me. The question remains what treatments are available that could help to repair this peripheral nerve function.
L says
Evidence of small-fiber neuropathy (SFN) in two patients with unexplained genital sensory loss and sensory urinary cystopathy. 2017
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5999027/
In both men, microscopic examination of PGP9.5-immunolabeled thick sections from a standard 3 mm punch skin biopsy to a depth of 2 mm (Fig. 1) from the distal leg (10 cm above the lateral malleolus) showed 148 and 117 neurites/mm2, corresponding to the 2nd and <1st percentile of expected values for individuals matched by age, sex and race for Case 1 and Case 2 respectively. Case 1 additionally had punch skin biopsy of the thigh (20 cm distal to the anterior superior iliac spine), which showed 68 neurites/mm2, for which there is no available normative data, though clearly abnormal as it is shows less epidermal nerve-fiber density than the distal leg, thus supporting the diagnosis of a non-length dependent small-fiber neuropathy.
Quantitative sensory testing cannot differentiate simulated sensory loss from sensory neuropathy. 2003
https://www.ncbi.nlm.nih.gov/pubmed/12578928
Anon says
Has anyone tried going back on the medication slowly to see if it improves any symptoms? I know most people wouldn’t want to since it’s the offending party but I’m curious if anyone’s tried.
Dr. David Healy says
We will have an interesting post about this on RxISK in 2 weeks time and will be asking whether anyone else has had a similar experience to the one the post outlines
DH
Laura Littleton says
Came here for looking for answers and hope. Started with cold burning, pricking, pinching pain in my feet and hands, mostly, but the cold burning fleeting in various parts of body, including legs, trunk and face. Thinking it may of been a withdrawal symptom from cold Turkey stopping Viibryd, I went on a low dose Lexapro after 4 months of suffering to see if it would stop. And it did! For about 4-5 months. But now it’s back. And with a vengeance. Upped my Lexapro dose to see if it helps. Jury is still out.
Anon says
Upon reducing Prozac 10mg over several months I developed classic withdrawal symptoms of insomnia, rebound anxiety/depression, nausea, diarrhea, etc so I reinstated 2mg immediately, and increased to 3mg after a couple months. As the classic wd symptoms have let up, the allergic type responses have ramped up, and I developed red blotches/inflammation on my joints (mostly fingers and toes) with burning pain that resemble urticaria, and I’m extremely sensitive to hot/cold. I suspected that I triggered an autoimmune inflammatory arthritis with allergies/ hives since my joints hurt/burned but the Rheumatologist suspects allergic urticarial vasculitis, and/or “small fiber neuropathy, which can cause pain overlying the joints due to nerve pain rather than arthritis.” The interesting thing is that I’ve gotten a more minor version of this when I tried to reduce Prozac in 2018 (red burning joints but on right hand, allergies, sensitivity to hot/cold) but it eventually went away slowly after I reinstated the full dose and by around 9 months I only had some persistent food sensitivities left. This time (2021) although I reduced slower, the burning pain is more severe & can’t hardly type, walk or write without pain. I didn’t reinstate the full dose this time, and it’s still spreading to more joints but I am thinking to try and reinstate gradually since I know it eventually let up after reinstating before. I don’t want to be on these drugs especially after already surviving the hell of acute classic withdrawal for months but it might be better than being disabled which is literally where I’m headed. It also may not work and I may never know if it does resolve, if it would have on it’s own and be stuck on Prozac but it’s looking like the least worst bet. My GP, Rheum & Psychiatrist have never heard of anything like this in withdrawal is there anything I can give them from you guys that might help?
Dr. David Healy says
Dear Anon
This is grim – no-one has any good answers for anyone else when withdrawal becomes as difficult as it has become for you. The option to try before re-instating might be to see if your doctor will switch you to imipramine – the rationale here is that its a gentler serotonin reuptake inhibitor than prozac. Difficult to know what dose to suggest -if you are only on a low dose, perhaps try 10 mg BD. But not clear what dose you are currently on
DH
Charles says
My twin brother got PSSD from an antidepressant sometime over the last two years, which got me interested in looking into it and finding solutions. It was strange because it sounded like a problem I had and still somewhat have now. Years ago, I was given Septra for an infection. I had a psychological reaction where nothing stressed me out and other people noticed I had weird expressions on my face. On the third or fourth day, my skin got loose where It looked like I got spontaneously fat for a couple hours. I developed some global numbness where the clear-ness of touch is reduced, I can still somewhat sense it, but it isnt as strong as before.
My thought was that it was an autoimmune reaction that partially effected mylein, the spinal cord, and/or the brain. Could this also be small fiber neuropathy? Is there a way to heal small fiber neuropathy that patients could try in experiments? There are so many new chemicals and growth factors being discovered that heal/repair nerves like BDNF, NGF, CNTF
Pamela Skewes-Cox says
April 6, 2022
I have been reading through all of these comments. Can anyone give me information on going back on the anti-depressant ( I was on Sertraline), to see if the symptoms of neuropathy go away? I very carefully weaned myself off of it over a period of 5 months ( I had been on it for almost 20 years). 3 months later, my feet went suddenly numb as if they had fallen asleep. Now it is almost 8 months later, the tingling and numbness is worse, sometimes moving up my legs and very bad at night. Is there any research on this option: to go back on the anti-depressant? Thank you, Pamela in Boston
Dr. David Healy says
Pamela
No-one can answer this – if you do go back on sertraline can you let us know what happens.
D
Laura Littleton says
I made a similar comment above. But going back on a different low dose SSRI got me 4-5 months of relief. My symptoms returned so we have upped my dose to see if it helps. Was on Viibryd. Now on Lexapro.
Vlad says
I have been enduring pretty much all of these symptoms for 6 months now after withdrawing from an AP called Rexulti as an adjunct to Moclobemide. I was on the Rexulti for 2.5 years and stopped after it was worked out that my delayed onset sexual dysfunction and severe RLS and sleep paralysis (18 months after starting) was from that drug. I was fine for 9 weeks after stopping apart from normal expected withdrawal, then numbness and burning started in my right foot and rapidly traveled upward to my saddle and genital area. Then weeks later my forearms and hands and face, tongue, jaw became numb and painful and eventually the whole body I then developed urine retention, and feeling of needing to pass No.2 all the time. Weeks later I couldn’t walk properly and move my hands without weakness and tremors. I had totally numb penis glans and soft glans syndrome despite return of normal sexual function after stopping Rexulti.
The symptoms kept getting worse, like extreme anxiety, weeks of insomnia, non sweating hands and feet. Swallowing and breathing issues.
I re-instated the drug at a low dose of 0.25mg 3 months and re-tapering off again but much slower. I have improved a lot but have worsen again on a recent reduction to 0.125mg. Not as bad as the first withdrawal but similar symptoms.
A few threads on the PSSD forum are finding links to SFN damage from autoimmune triggered by SSRIs and other medications. I am going to ask my doc for biopsy and if available here in Aus, blood tests for Anti-TSHDS-IgM-Antibidies and anti-FGF Receptor- 3 antibodies. A member has tested positive and others are looking into it themselves.
Dr. David Healy says
Keep us posted on the results of any tests
If there are people with PSSD who have positive test results can you let us know this could be a really helpful lead.
But bear in mind, Covid vaccines can cause some of these symptoms and test changes also. There is a striking overlap in fact.
Rexulti and Abilify can cause terrible problems
D
Longterm says
I think neuropathy is obvious in “pssd” and other syndromes with same symptoms. In addition to bodily/autonomic neuropathy some fragile types of cells get injured in brain too.
All research efforts should be focused on the microscopic nature and causes of such damage (involving drugs and not) . All other research at this point is just useless in my opinion.
Matt Plahuta says
I have many of these symptoms. I took Lexapro 18 months ago, for 10 days & quit after experiencing horrible symptoms. 18 months later & taking no medications for entire 28 months, I still have symptoms. Tinnitus, full body neuropathy, ED, loss of taste/smell, no energy, fatigue, blurred vision, memory loss, trouble thinking, emotional numbness, body temperature dysfunction & more. I believe all neurological & all caused by Lexapro. Has anyone found anything that helps these symptoms? I’m planning to do a sauna detox program & hope it helps.
Peter Winkler says
I have a lot of symptoms like that too I am taking cymbalta and I am having brutal withdrawal symptoms . I am tapering super slow . Taking out beads…
Did you find any solutions or we have to live our life like this now ?
Thank You.
Louise says
Wow. So this evening I’m googling SSRI withdrawal and nerve damage to try and find an answer to why, 3 months after tapering off of 8 years of 15 different brands of antidepressants and benzodiazepines, that I am experiencing extreme pain, burning and cold sensations from my pelvis down, but mainly in my lower legs and feet. Like intense foot cramp you’d get if you wore a pair of ski boots that were too small for you. Calf and quad cramps. Pins and needles. Sensitive to hot and cold temperatures. I had to stop in the street yesterday and hold on to a bin to steady myself.
Since tapering off of my meds ( because I was diagnosed in Oct 2022 with Treatment Resistant Depression). I am having a rollercoaster of:
– emotions, good and bad. A LOT of crying.
– brain zaps which the neurologist doesn’t understand and almost looks at me as though I’m speaking another language when trying to explain them
– migraines with aura. 14 in the past month
– blurred vision
– cognitive function issues
– poor short term memory
– increased anxiety
– smell and taste changes. I can no longer eat many types of fish I used to enjoy
– loss of appetite (I’m ok with that, I gained 30kg over 8yrs on antidepressants)
I did have loss of sensation in my genitals for years on SSRIs, but that’s slowly coming back.
Went to my doctor today re the pain I’m experiencing in my legs and mentioned could it be related to my SSRI withdrawal and linked to all the migraines, and a type of concussion I had without an impact a few months back. A nervous system issue. He said I have a temperature and probably it’s a viral infection causing the leg pain, but come back in 2 weeks and maybe he’ll investigate further into G&B syndrome if it persists.
Lying here I want to scream that doctors are just ignroing the effects these medicines are having/had on us. I also got non alcoholic fatty liver from the Escitalopram days and the head zaps were my own phenomenon according to the doctor.
I am certain that my blood pressure and body temperature increased due to SSRI’s. I was diagnosed by another neurologist with Carpal Tunnel and recommended to have the operation in both hands. I politely declined and noticed that if I cut out as much gluten and starch sd possible it helped, though that’s hard when you have Major Depressive disorder and want to eat too because the SSRI’s make you constantly hungry.
Post SSRI’s I am eating a plant based (real, not packaged) diet. I don’t drink alcohol, I exercise gently daily. At least 30mins walking. I’ve dropped 7kg in 3 months, but I’ve a long way to go.
Pressured my doctor into giving me a full spectrum blood test next week – as I want to see if I’m deficient in anything.
Any direction on support / patient groups would be most welcomed. I’m over it!
Thank you and especially to all of you that are continuously researching ways to help people like me and others in this group.
Laura Littleton says
I am also cutting out gluten to see if it helps. I will try anything.
Emily Ruck says
Hi.
I’m a 27 year old female from wales and I think I have this . I have a burning sore achy sensation in my scalp and head whenever someone touches me or massages me and whenever I eat a nice meal. I cant feel pleasure just an uncomfortable altered sensation in my head . I also cant orgasm or feel pleasure from sex or cuddling . This has taken its toll on my mental health and well-being . I am usually a quite a jolly and optimistic person . Since I developed this symptom I have been sad hopeless and pessimistic
Emily Ruck says
I wonder if there is a cure for this small fiber neuropathy . This describes perfectly what i have and suffer from on a daily basis
Emily Ruck says
I have this intense burning tingling altered sensation in my scalp and head . For me this is unbearable and I cannot live with it . I cant feel pleasure from anything I do including sex and eating and my quality of life is very low . I dont know if there is a cure for it
Jay says
I have confirmed SFN (skin biopsy) and EM from very short term prescribed benzo use (5 months of xanax at .5 mg for sleeping). This shows up in benzo cases as well. Cannot walk and it is moving up my legs. Bedridden and completely debilitated. Will be heading to Switzerland for assisted suicide. I was an extremely healthy, extremely active individual before taking xanax. Primary doctor did not provide informed consent and I had no idea what I was getting myself into. My life has been destroyed and I suffer 24/7. Have not slept more than 2 hours a night since. Pegasus in Switzerland will approve this type of condition for assisted suicide. I am working through the application process right now. I have no idea how people live with this.
U says
Jay
Is it only neuropathy or are you suffering from akathisia as well? F*cking benzos leave people with akathisia upon stopping. I don’t know if it ever stops. Please wait for a second.
I am extremely sorry and heart broken to read your comment. I have been luckier than you in a certain sense that I have half-survived the 8 years of copious amounts of psychotropics. The 6 years of it was very high doses of experimental medicine combinations. I REALLY KNOW how painful it can get and I am on the edge of taking my life as well. From bladder problems to sexual dysfunction, constantly passing gass like a f*cking fart machine, night sweats as if I took a dip in a swimming pool, itching that keeps me awake at night and crippling anxiety that was NOT a part of my original condition, before I was run through these medicinal experiments by greedy idiots, all without my consent. I am constantly on survival mood since february 2013. All these health problems despite not drinking, smoking, working out and living healthy… THIS IS HELL.
But, could you please, for this stranger that answered to you, somehow wait a bit longer and try other things? Can you please try to book an online consultation with David Healy or something? It would be quite expensive but this is something that you can do to get some answers before you end it all. PLEASE? I mean why do you have to die? Why are you getting punished as an innocent person who got scarred by some bastards? Please, try changing your life drastically if it’s possible? Get enrolled in military? Man I don’t know, flee to the country side, sleep on the fields, try alternative medicines, try even medicines that are not legal?
Pick some f*cking god, spirit, anything and pray. Breathe. Man I mean, I was looking up how to apply for medical assistance in dying myself yesterday but why do WE have to die? Please! Look at the mirror and try to remember your childhood. Imagine that an innocent child like that came to you, scarred and crippled by a stupid doctor and he is in pain. Would you try to save him and ease his pain or put his life to an end?
VERY IMPORTANT: 1. DON’T CONTACT A PSYCHIATRIST 2. DON’T GO TO A PSYCHIATRIC HOSPITAL 3. CUT OFF CAFFEINE, ALCOHOL, ANY SORTS OF MEDICINE AND PAINKILLERS IMMEDIATELY. 4. CONTACT SOME RELIGIOUS / SPIRITUAL GROUP OR PEOPLE, PREFERABLY HIPPIES.
I LOVE YOU STRANGER PERSON. YOU DESERVE LIVING. WE DESERVE LIVING. LET ME KNOW.
U
U says
Jay
I posted a very long answer to your comment, missing the part about “Cannot walk and it is moving up my legs. Bedridden and completely debilitated.”. I managed to miss that detail in the heat of all emotions. So my first answer to your comment won’t make so much sense if it gets approved by the moderation. I don’t know what to say. Hopefully you won’t get upset at my answer. I wish the best for you. I wish you can find the patience and the power to stay around a bit longer to hopefully find a cure or treatment. I hope you will be okay.
U
Kim Ambs says
I am going through this right now. Red numb foot. Red goes up to knee. Trying to come.off Cymbalta 😢
Justin Butcher says
This is an interesting study on drug induced neuropathy on pubmed
https://pmc.ncbi.nlm.nih.gov/articles/PMC7365998/
I have neuropathy discontinuing Depakote 750mg daily over 12 years
Justin
Dr. David Healy says
Thanks for the link. It steers as far away as it can from mentioning the link to SSRIs SNRIs and other commonly taken medicines probably because no journal would publish something linking serious hazards to our favorite sacraments
D
Justin Butcher says
Just to say it taken 4 years to come off the depakote. Been off it 1.5 years. Thanks for the reply