This post is about you who read it, and the ten of us or so who have helped write it, having an impact on the system. Modern healthcare is very disempowering. The arrangement that makes some medicines Prescription-Only began life as a police function and unfortunately many of us consulting a doctor can feel knee-high to a policeman especially if we even begin to hint that a treatment may not have turned out absolutely perfectly. If we get to check our medical records we often find that this has led to records we view as wrong.
There are many RxISK posts on the theme of how to get incorrect diagnoses or details in our records changed – see Changing a Medical Record 1, and 2, and 3, and 4. It’s very difficult, almost impossible. For many of us, its not just that the medical record is wrong, the system has captured our identity – the person there is not us. See all the posts with a Medical Kidnap label.
A door, however, might just have opened up. Doctors only want medical things in medical records and figure when you talk about things like PSSD or protracted withdrawal that you are talking internet gobbledegook. But PSSD and protracted withdrawal now have medical codes. They are as much a part of medicine as heart attacks and strokes.
Read on.
A Door Opens?
Last week we ran a post – MHRA Adopts Code for Post-SSRI Sexual Dysfunction. Could this be the first stone that triggers an avalanche? For the first time, it’s possible to officially report post-SSRI sexual dysfunction (PSSD) to the UK’s drug regulator, the Medicines and Healthcare products Regulatory Agency (MHRA). This is because they have started using a MedDRA code for the condition (10086208) that was introduced in 2021. Other regulators are likely to follow suit.
If regulators across the world were to start receiving large numbers of reports for PSSD in this way, it will put pressure on them to do more in terms of providing better warnings and increasing awareness among healthcare professionals.
Its worth reading last week’s post. MedDRA is a coding system regulators created to code the side effects of medicines.
A number of dedicated patient activists heavily involved in PSSD, protracted antidepressant withdrawal and other adverse effects, have recognised the importance of this development and suggested ways to take it further. It was a comment from Harriet on the post that really set the ball rolling.
Having an impact
A battle facing many sufferers of PSSD, protracted antidepressant withdrawal syndrome, and other side effects from antidepressants like visual snow syndrome (VSS) and persistent perceptual postural dizziness (PPPD), is that without a sense that medicine in general recognizes these as established adverse effects, doctors may be slow to accept your symptoms as drug-related and very reluctant to record them as such in your medical record.
Our 2019 journal article on PSSD patient experiences highlighted some of the reactions that patients receive. See also It Feels Like We’ve Been Lobotomised.
When RxISK was first launched, our main initiative was the RxISK Report. This is a detailed document that you can fill and receive a score to indicate how likely it is that your problem is caused by a medication you are currently taking or have previously taken. The idea was that you could take the report to your doctor, and it would support the conversation you needed to have with him/her and hopefully persuade them to take on board what you were saying.
While several thousand patients have completed RxISK Reports, the feedback suggests very few of you have opted to take it to your doctor. This is understandable. Doctors are busy and appointments are brief. You need a lot of dedication to turn up with a RxISK Report and explain what it is, where it’s from, and what the doctor should do about it. The report is also several pages long.
RxISK reports have still be hugely useful in ways we didn’t expect. Anonymised data from them has formed the basis of several peer-reviewed journal articles including the article on diagnostic criteria for PSSD and other sexual dysfunctions that was published in 2022 (online in 2021).
The RxISK Report remains a primary feature of our website, but Harriet’s comment outlines something else that may be just as important and easier to manage.
Mark Horowitz launched the SNOMED component of this and the PSSD Network had the MedDRA idea.
Harriet’s idea stemmed last week’s post – the introduction of SNOMED codes for PSSD (SCTID: 1340196008) and protracted antidepressant withdrawal syndrome (SCTID: 1285639002). SNOMED is used by doctors and medical practices to record medical conditions in the notes.
She suggested a one page form that anyone reading this could fill in with a few basic details including the appropriate SNOMED code, ask for the relevant SNOMED code to be recorded in your notes and this letter to be placed on your medical file. See below.
While a doctor might be reluctant to acknowledge these conditions during a face to face meeting and record them in the notes, simply filing a form that you have provided may seem more appealing to them. There is potentially no need for a face-to-face meeting – the form could be posted, emailed or hand-delivered to the clinic.
What’s in a name?
Antidepressant withdrawal as a concept is problematic for healthcare professionals. They are taught that withdrawal is something that lasts days or weeks, not something that a person can still be experiencing years after stopping the medication. The difficulties getting off antidepressants were always likely to lead to formulations stressing protracted withdrawal. The same holds true for benzodiazepines, antipsychotics and mood-stabilizers.
A quarter of a century ago, a Pharmacological Stress Diathesis Syndromes paper outlined what is now increasingly accepted is happening. The idea is also embodied in a set of RxISK guides on Stopping Antidepressants, as well as stopping antipsychotics and mood-stabilizers (which has linked posts on withdrawal and stress syndromes) written over a decade ago, last updated a decade ago, in need of further updates but still valuable.
Up until recently, a recognition that withdrawal could be protracted could only be found in patient groups and internet forums. Then tapering and hyperbolic tapering came along and there is a growing acceptance of the real state of affairs in professional bodies and guidelines.
The introduction of a SNOMED code for protracted antidepressant withdrawal syndrome adds a significant dollop of legitimacy and in particular makes it possible for your view of what is happening you to get formally recorded as a medical condition in your healthcare record.
The SNOMED description notes: “Antidepressant withdrawal may last for 2-3 weeks but can transition into a protracted withdrawal syndrome (PWS), which can last many months or years.”
People with PSSD often have other accompanying non-sexual symptoms, and these can now be recorded using the SNOMED code for protracted antidepressant withdrawal syndrome. For example, if you have gastrointestinal problems in addition to PSSD, you could describe yourself as having both PSSD and protracted antidepressant withdrawal syndrome.
Ideally, however, it would be better to find all of the SNOMED codes for your specific problems eg. gastroparesis, interstitial cystitis, akathisia, etc. We will have to find out if it’s possible to get specific codes for drug-induced or SSRI-induced VSS or PPPD, etc.
This offers all of us a chance to be a nuisance – a nuisance that the system cannot afford to dismiss.
How to find a SNOMED code
SNOMED is an international set of codes, so anyone reading this from almost anywhere can start to play the system. This History of SNOMED – tells you what it is and where it comes from.
We sent the most tech illiterate of our team to see if he could find some codes – and he did. If he can, so can you.
Go to this link for the SNOMED browser.
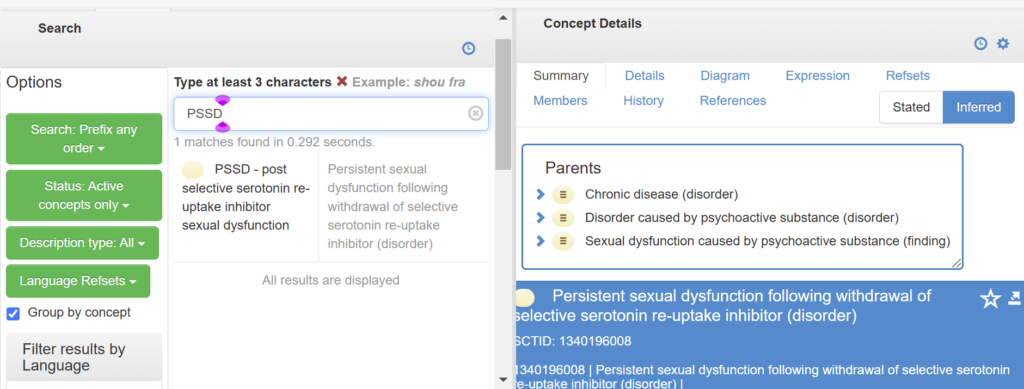
The search box and concept details box will be empty.
Typing PSSD into the search box brings up the text below it. Clicking on this PSSD text brings the code and concept details into view on the right-hand side in the blue box.
The text in the blue box is interesting and useful. There is much more there than you see on this screen. It makes clear that this is a drug-induced condition – no ifs, buts or maybes.
Typing protracted antidepressant withdrawal syndrome brings up this condition and, again, the concept details are useful.
At the moment, typing protracted benzodiazepine, antipsychotic or anticonvulsant aka mood stabilizer withdrawal into the box brings up nothing.
There are codes for:
- Visual snow syndrome SCTID 771237009
- Persistent postural perceptual dizziness SCTID 103293001
- Interstitial cystitis SCTID 38731000087104
These can all feature as part of the protracted withdrawal picture. They may start on treatment before you withdraw, but almost all the features of protracted withdrawal are also essentially there before you start withdrawing. The codes at present for these and other problems do not say drug-induced.
SNOMED has very few specific prescription drug-induced codes. PSSD and protracted withdrawal are helping break this mold. See Tim’s comment on last week’s post – he will be pleased to know there is one for drug-induced akathisia SCTID 230333002.
Akathisia, like PSSD can almost only be caused by medicines. We figure there are over 500 drugs that can cause it including antibiotics, hormones, all psychotropic drugs and others – see drug-induced akathisia link.
There are however some other drug-induced problems with SNOMED codes including:
- Drug-induced sleep disorder SCTID 418475009
- Drug-induced constipation SCTID 21782001
- Depressive disorder caused by drug SCTID 191495003
- Mood disorder caused by drug SCTID 429672007
The current code for PSSD is tied to serotonin reuptake inhibitors. We may need a separate code for drug-induced enduring sexual dysfunction that could be applied to mirtazapine which also acts on the serotonin system and gives a close to identical picture in terms of sexual dysfunction to SSRIs.
This brings up the need for codes for the enduring sexual dysfunctions linked to isotretinoin and finasteride. Although not specific to sexual issues, we found:
- Isotretinoin adverse reaction SCTID 292669009
- Finasteride adverse reaction SCTID 293228002
SNOMED has Request Submission Portals. If you google SNOMED, you will find there is access to a bunch of systems from Argentina to the US, each of which will have a health organization licensed to use SNOMED. In the UK, there is a portal linked to the National Health Service which has a license – which is in the link above.
Whether in the US or Argentina, it looks like you will need friendly doctors to log in and make a brief 300 word submission that makes a case for Code X for Condition Y. This will likely be something you or we write for them. Here is the Submission for PSSD.
There will be something similar in other countries. Please send us details if you find links to the right portal for you and if you can recruit a friendly doctor to help.
Your input
In terms of moving things forward, our initial thought is to put together a PDF form or Word document on the RxISK website that you can print off and complete. Harriet suggested something like this:
Heading: Please ensure and confirm that the following essential information is entered into and attached to my medical records. Thank you.
- Surgery name
- Patient name
- NHS number (UK only)
- Patient contact details (email, phone)
- Drug(s) causing ongoing adverse reactions
- Date started
- Date stopped – or still tapering for (number of months)
- Adverse reactions experienced
- Diagnosis based on drug/symptomology
- System codes – SNOMED SCTID XXXXXXX, (MedDRA – if you have it)
- Signature, date
Your covering note should try to make it clear to the clinic you want a SNOMED code put in your record and ideally also want your letter attached to your record.
Harriet thought including publication details of a few references might help get the doctor onside but this is not necessary.
Pushing this door open needs your efforts with your doctor and you sharing any thoughts and ideas while you do it.
Let us know about any SNOMED and MedDRA codes you find not listed here. It would be great if you could add them in a comment on this post or email them through Contact RxISK.
One of the useful things about MedDRA codes is that they can all, pretty well by definition, be drug-induced.
We will set up a resource on the RxISK website in the Guides and Tools menu listing all the SNOMED and MedDRA codes that you send us and that we can find, and once it’s up and live we will add a link here. We will also list all other coding systems you may have heard about – DSM, ICD and others that might be helpful.
Update: The Healthcare Record Pro Forma is now available.
Hilarious
There was a moment of hilarity during the writing of this post. One of us, not Harriet, consulted CHATGPT for its views on PSSD and found the following.
Chat GPT November 30 2024
Post-SSRI Sexual Dysfunction (PSSD) has been recognized as a medical condition and assigned the MedDRA (Medical Dictionary for Regulatory Activities) code 10086208. This code facilitates its identification and reporting in pharmacovigilance systems globally. MedDRA is widely used in regulatory contexts to standardize the classification of adverse drug effects, which helps in recognizing and addressing conditions like PSSD. rxisk bmj
If you’re reporting or researching this condition, referencing this code can ensure consistency and better visibility in medical records and studies. For additional context or updates, it is also helpful to consult regulatory bodies such as the European Medicines Agency or organizations like RxISK, which document and advocate for awareness of PSSD.
(It includes this link which takes you to Harriet – pslhub)


Nick A. says
Good to see you’re finally recognized by big AI as a regulatory agency.
What would you say to those who are worried about arrogant/stubborn doctors regarding reporting this condition? Should they just try to find a friendlier doctor should they not at first succeed?
Dr. David Healy says
I would change doctors rather than give yourself too much grief. Always good thought to appeal to their better nature if you can rather than argue with them or try to educate them how to practice medicine.
D
Nick A. says
Thanks for the info. I’ve coincidentally got an appointment tomorrow and I am hesitant to even try because in the past he’s said that *all* sexual symptoms of antidepressants are psychosomatic. Verifiably insane take
tim says
SCTID 230333002 So there is a code for DRUG-INDUCED AKATHISIA.
Accurate and committed coding clarifies (or should clarify) the prevalence of this potentially devastating adverse drug reaction.
Yes, I am pleased to read this, however, having tried to raise awareness of akathisia via letters and rapid responses in medical journals for many years, it is perceived that there is a greater professional emphasis on akathisia denial than on akathisia recognition.
How can reliable and reproducible coding be achieved for a condition that remains vulnerable to denial, misdiagnosis and failure of prescribers to recognise?
chris says
For a while I’ve been doing a search on akathisia on the NHS website so far nothing comes up:
https://www.nhs.uk/
It’s shocking !
chris says
RE: https://www.dailymail.co.uk/news/article-14153367/Lady-Gabriella-Kingston-husband-Thomas-died-shotgun-wound-medication.html
A major result for the truth but devastating for the family. I hope Lady Gabriella and his family can set up a situation that will help prevent this. They certainly have the power to influence the situation.
Don’t know if they already knew you David but when I first heard about this case I sent a message via the Palace website saying if he had been prescribed psychotropic medication it could be akathisia and that you were a world expert in adverse drug reactions and the person to speak with about it, and forgot about it thinking it would be ignored as all my many other emails to mostly editors have been.
Looks like someone actually took note.
annie says
By KATINKA BLACKFORD NEWMAN FOR THE DAILY MAIL
Published: 20:33, 12 June 2023 | Updated: 11:53, 4 December 2024
Taking antidepressants led our loved ones to take their lives: Grieving parents tell of their agony – as experts reveal what every person prescribed them should know about the risks
For confidential support, call the Samaritans on 116 123
https://www.dailymail.co.uk/health/article-12186777/Agony-families-say-pills-depression-led-children-lives.html
All grief can cause complex feelings — but losing someone to suicide comes with a particular sense of agonising regret, powerlessness and unanswered questions.
The knowledge that a prescription drug might be the cause can only exacerbate that pain, particularly if the prescribed drugs in question are antidepressants — pills that are supposed to prevent people from feeling suicidal.
Tania and Ian Morgan, from Swansea, lost their 25-year-old son, Sam, when he killed himself in January 2020. They believe his death was caused by an adverse reaction to an antidepressant.
‘Sam had everything going for him,’ says Tania, 59, a head teacher. ‘He had a steady girlfriend of six years, no financial worries and a group of fantastic friends. He was a junior trader for a financial company and had a great future ahead of him.’
Sam had been taking the antidepressant citalopram for seven days prior to his death. Citalopram is a type of antidepressant known as a selective serotonin reuptake inhibitor (SSRI), which is thought to work by increasing serotonin levels in the brain.
While antidepressants can be life-changing for many, there is evidence that they can raise the risk of suicide, with experts arguing they can even make people who aren’t depressed feel suicidal.
A significant piece of research published in April 2023, in the journal Ethical Human Psychology and Psychiatry, raises doubts as to the efficacy of antidepressants, as well as adding to concerns that these pills may increase suicide.
The study looked at nearly 8,000 reports from coroners’ inquests in England and Wales between 2003 and 2020 where antidepressants were mentioned and found that around half of the deaths were definitively ruled to be suicides.
The study author, John Read, a professor of clinical psychology at the University of East London, concluded: ‘We do not know in how many cases the problems for which the drugs were prescribed contributed to the deaths. Nor can we tell in how many of the 7,829 cases that antidepressants contributed to the deaths.
‘We can say, however, that antidepressants failed to lift the depression sufficiently to prevent these deaths.’
The study was based on research by a grieving father, trying to come to terms with losing his ‘happy-go-lucky son’, who killed himself after taking the antidepressant drug citalopram.
The father, Brian, who wishes to give only his first name, was convinced his 30-year-old son’s death in 2009 was caused by an adverse reaction to the drug.
‘He had everything going for him and wasn’t depressed,’ he told the Mail. ‘He loved life. He was just a bit stressed at work and couldn’t sleep.’
After his son’s death, Brian began studying newspaper reports of inquests in England and Wales where antidepressants were mentioned and posted them on his website AntiDepAware. His findings were then analysed by Professor Read, who concluded in his report that the figures were likely to be the tip of the iceberg, as many suicides and inquests are not reported in the media.
One in six people in England (8.32 million) took antidepressants in 2021/22, a 5 per cent increase from a year earlier, according to NHS data.
Not all will be taking them for depression, as antidepressants can be prescribed for many other conditions including eating disorders, mild anxiety and pain relief.
Since 2004, all antidepressants have carried warnings on the information leaflet in the packet, explaining that if you have suicidal thoughts these may increase when you first start taking the medication because they take a few weeks to work. Some experts believe the wording is inadequate and misleading. David Healy, a former professor of psychiatry at the University of Wales College of Medicine, has worked as a consultant to pharmaceutical companies who make antidepressants.
He has been writing to regulators and coroners in the UK for 24 years about the need for clearer warnings. ‘As far back as the 1990s, it was well known among the drug companies from the clinical trials that antidepressants can directly cause even healthy people to commit suicide after they’ve been on the drug for a few days,’ he told Good Health.
He describes how these drugs can cause intense agitation and emotional turmoil in some — ‘yet calm others down’.
‘This is because our serotonin systems differ,’ Professor Healy says. He is routinely contacted by grieving families of people who have taken their lives and who believe that depression medication was a possible cause.
Tania and Ian Morgan found Professor Healy through an internet search as they struggled to make sense of their son’s death. Sam had not been depressed when he visited his doctor in January 2020.
‘Over Christmas, he had a persistent cough and had been unable to revise for his financial advising exams so he went to see his GP to get a sick note for the examination board,’ says Tania. ‘He also mentioned that he was feeling nervous about his exams.’
Sam asked the doctor if he could have some citalopram.
‘He knew about it because a friend had taken it and said it helped with her anxiety,’ says Tania. ‘Yes, Sam was nervous about his exam but that was just normal levels of stress.’
In a consultation that lasted ten minutes, Sam’s GP prescribed him a 14-day course of 10mg of citalopram, the lowest dose.
After Sam’s death the doctor told the Morgans that he didn’t want to give Sam the tablets because he didn’t feel he needed them but Sam persuaded him.
The GP also gave Sam the standard advice — that the tablets might make him feel worse before he feels better. Sam lived at home and his parents noticed a difference after he had taken just one dose.
‘There was an instant change in his mental state,’ says Ian.
This is what convinces the Morgans, like other bereaved families, that it was the drug, not their loved one’s mental state, that made them suicidal.
‘He just seemed apathetic and as if he’d given up on life,’ says Ian. ‘He said he felt sick and was unable to sleep. There was a greyness about him and his eyes were just dead.
‘Overnight, he had gone from being chatty and cheerful to being morose and like a zombie.’
Seven days after Sam had visited his GP, Ian saw his son for the last time.
‘It was in the morning and I was getting ready for work,’ says Ian, 59, a retail sales consultant.
‘I passed Sam’s bedroom and he said he felt sick and hadn’t slept so was going to take the day off. I asked if he wanted to put the heating on and he said yes.’
Tania came home later that day to find her son dead, a scene that will forever haunt her.
‘It was total shock and disbelief. I can’t begin to describe it. I felt totally numb,’ she says. ‘Sam was the last person in the world to kill himself.
‘Firstly, we wondered if there was something going on in his life that we didn’t know about, such as financial problems or a gambling addiction — but there was nothing. The only thing that had changed recently in Sam’s life was that he had started taking antidepressants.’
Their suspicions were confirmed when they contacted Professor Healy and showed him Sam’s medical records.
‘There was no reasonable explanation for why this young man ended up dead a week after beginning on this drug other than the drug had caused the problem,’ says Professor Healy.
The Morgans want to prevent other lives being lost.
They were frustrated that at the inquest the coroner ruled a narrative verdict (which records the factual circumstances of a death only, without attributing a cause), saying that ‘the effect of this medication [citalopram] on Sam is unknown’ and were disappointed that the GP’s legal team dismissed the link between the drug and Sam’s death.
However, Professor Healy believes that doctors are reluctant to speak out about the potential harms of medication because they are advised by medical insurers that it may put them at risk of litigation. This makes it hard to bring about change. ‘If doctors admit that the drug caused the problem, then the MHRA [Medicines and Healthcare products Regulatory Agency] have to sit up and take notice and do something to warn the public by requiring drug companies to make their warnings clearer,’ says Professor Healy.
The Morgans agree that current warnings in the patient information leaflet, which are written by drug companies and approved by MHRA, are both misleading and not prominent enough.
‘Buried in 3,000 words about citalopram there is a warning in the small print that if you already have thoughts of killing yourself then these may become worse,’ says Ian. ‘If Sam had known that the drugs were actually making him feel suicidal, he would probably not have continued taking them and he would still be here now.’
Professor Healy adds: ‘The wording needs to explicitly say that these drugs can directly cause suicide even in healthy volunteers taking them. If you feel strange or agitated, stop taking them. There will always be another antidepressant from a different class that will suit you better.’
This wording should also be somewhere obvious, he suggests.
Separately, Professor Healy thinks that telling patients that the drugs can take weeks to work could be costing lives — for while your illness might take time to respond, patients should be warned explicitly that they should not feel worse in the interim.
‘An adverse reaction to antidepressants can happen within hours,’ says Professor Healy. ‘People describe an agitation that they compare with being on the 55th floor of a building with flames surrounding them and it’s more comfortable to jump off than endure the agony. This uncontrollable urge to kill yourself is quite unlike depression.’
Professor Healy saw this at first hand when he ran a trial of the antidepressant sertraline in North Wales back in 1999.
None of the 20 volunteers had any mental illness — but after just a few days two of them, women in their early 30s, became suicidal. One was a doctor, the other was an administrator.
Professor Healy has agreed to share extracts from their diaries, kept as part of the trial, with Good Health.
One wrote after four days: ‘I know with absolute clarity and certainty that I had to go through the door out to the road and wait for a car. It had to be very final. A car or a train but a car was the overwhelming image. Yes, it would be violent but that was vital and necessary.’
Another volunteer wrote after ten days: ‘I must admit I have nightmares, the same one [on] two consecutive nights where I’m hanging myself . . . in our bedroom.’
Doctors read the diaries daily and both volunteers had to be taken off the trial for their own safety. Neither had ever felt suicidal before taking the drug and haven’t since. The power of antidepressants to cause people who aren’t depressed to want to harm themselves is something I have experienced personally.
In 2012 I was struggling with insomnia while going through a divorce and visited my doctor for sleeping pills. Instead, he prescribed the antidepressant escitalopram, which triggered a four-day delirium during which I hallucinated about how to end my life.
Admitted to a private hospital, I returned to normality after a few days once the drug wore off. Yet the doctors insisted I’d had psychotic depression, and gave me more antidepressants and also antipsychotics, triggering another adverse reaction and a year-long, drug-induced illness.
One symptom of drug-induced suicidality is an agonising condition, akathisia, a movement disorder where you cannot keep still and are seized with an inexplicable acute anxiety: I suffered from this on and off for a year.
Looking back, it was a miracle I didn’t end my life. I completely recovered within three weeks of finally being taken off all six drugs I had been prescribed. That was ten years ago; I have been medication-free and have not had mental health problems since.
My terrifying ordeal with antidepressants led me to write a book — The Pill That Steals Lives — and set up a website, anti depressantrisks.org. As a result, I’m contacted by many others with similar experiences.
One of these was Tara Baker, a catering assistant from Pembrokeshire, who considers she is lucky to have survived her experience with antidepressants.
Like many, she was struggling with the effects of Covid on her mental health when she went to her GP in March 2021.
‘I just felt anxious about not being able to go out and the fact that my little boy was coming up to nearly two and I felt he’d missed out on so much,’ she says.
‘It was financial stress as well, as my husband had been made redundant. I wouldn’t say I was depressed. I was just mildly anxious and I couldn’t sleep properly.’
Tara asked her GP for an antidepressant: ‘A few of my friends were on them and I thought it would be a quick fix.
‘The nurse practitioner gave me a prescription for sertraline [a type of SSRI] after just a five-minute phone consultation.
Within an hour of taking the first tablet, Tara had an extreme reaction: ‘I felt really shaky, was having cold sweats and my pupils were huge.
‘I had these random intrusive thoughts about killing myself. It was as if a video was playing in my head. I went for a walk to calm myself down but then I just pictured myself jumping into the water.’
Tara continued to take the pills because she, too, had been told that she might feel worse before she felt better.
Her condition deteriorated and after three days of not sleeping or eating she contacted her GP who prescribed a tranquilliser, diazepam, and advised she keep taking the antidepressants.
After a week, Tara, who had never felt suicidal before, tried to end her life. She says: ‘My brain just wouldn’t stop. I just felt this unbearable agony and I wanted it to go away.
‘I know it sounds insane but I was convinced I was sacrificing myself to save my family so God would understand. I felt really out of it, as if I had no emotions.’
Fortunately, Tara’s husband came home in time and called an ambulance.
The crisis team at her local hospital recognised that she had an adverse reaction to the sertraline and told her to stop taking the tablets immediately.
Tara was so frightened that she asked to be sectioned but the doctors wouldn’t do this. She asked the crisis team to drive her to another hospital where she admitted herself.
‘I slept for 16 hours and when I woke up everything was OK — but I was still shell-shocked,’ she says. ‘I told one of the nurses that the antidepressants had caused this and she said it couldn’t be possible because sertraline takes three weeks to have any effect.
‘It took me a few weeks to feel completely normal but I think that was partly because of the trauma.’
It has been three years since Tara’s ordeal and she thinks she had a lucky escape.
‘I’ve still got a bit of anxiety about certain things, but I deal with it by distracting myself until it passes and by keeping myself busy.’
A spokesperson for the MHRA told Good Health: ‘Patient safety is our top priority. ‘We have kept the safety of SSRIs under constant review ever since they were first licensed. The available data continue to show that the benefits of SSRIs in treating depression and other psychiatric illnesses outweigh the potential risks for most people.
‘Following concerns raised by patients and families about the effectiveness of product information warnings, we have established a new independent expert group to advise the Government’s statutory advisory committee, the Commission on Human Medicines. This will consider whether changes are needed to the current risk minimisation materials for SSRIs, including the patient information leaflets.’
The spokesperson added: ‘Patients who have concerns should talk to their doctor and should not stop taking their antidepressant medication without their doctor’s advice.’
For confidential support, call the Samaritans on 116 123 or visit a local Samaritans branch. Go to samaritans.org for details.
Katinka Blackford Newman runs antidepressantrisks.org, a campaigning website that raises awareness about the potential risks of antidepressants.
chris says
So this is important by katinka, really gets at what is going wrong and what needs addressing urgently. For myself I see these as profoundly important:
“However, Professor Healy believes that doctors are reluctant to speak out about the potential harms of medication because they are advised by medical insurers that it may put them at risk of litigation. This makes it hard to bring about change. ‘If doctors admit that the drug caused the problem, then the MHRA [Medicines and Healthcare products Regulatory Agency] have to sit up and take notice and do something to warn the public by requiring drug companies to make their warnings clearer,’ says Professor Healy.”
“Separately, Professor Healy thinks that telling patients that the drugs can take weeks to work could be costing lives — for while your illness might take time to respond, patients should be warned explicitly that they should not feel worse in the interim.”
“In 2012 I was struggling with insomnia while going through a divorce and visited my doctor for sleeping pills. Instead, he prescribed the antidepressant escitalopram, which triggered a four-day delirium during which I hallucinated about how to end my life.
Admitted to a private hospital, I returned to normality after a few days once the drug wore off. Yet the doctors insisted I’d had psychotic depression, and gave me more antidepressants and also antipsychotics, triggering another adverse reaction and a year-long, drug-induced illness.”
This is incredibly important to understand.
“he prescribed the antidepressant escitalopram, which triggered a four-day delirium”
It’s usually the case that emotional lability comes first then akathisia then more drugs prescribed or forced and then toxic psychosis/delirium. But in this case Katinka seems to have had akathisia kick off very quickly followed by delirium and maybe toxic psychosis also quickly.
“Yet the doctors insisted I’d had psychotic depression, and gave me more antidepressants and also antipsychotics, triggering another adverse reaction and a year-long, drug-induced illness.”
This is the all too common disaster that is happening in psychiatry – identifying what is actually happening and therefore being able to help the patient who is usually in a terrible state. Psychiatrists are programmed to drug people severely agitated and going into self harm and violence through akathisia delirium and toxic psychosis to sedation. What needs to happen is padded rooms and people prepared to do one on one’s or more two or three people to be with the affected patient and no drugs but the patients own body helped to initiate GABA through the normal requirements of the body to eventually calm and stabilize them.
annie says
Daily Mail is running another article by Katinka, this evening
Antidepressants left me suicidal due to a little-known condition. Now after hearing other shattering stories I want to warn of the risks doctors tell me – and everyone should know: KATINKA BLACKFORD NEWMAN
By KATINKA BLACKFORD NEWMAN FOR THE DAILY MAIL
Published: 17:12, 4 December 2024 | Updated: 17:20, 4 December 2024
https://www.dailymail.co.uk/health/article-14157991/Antidepressents-suicidal-risks-doctors.html
She has written numerous letters including to the medical regulator, the MHRA (the Medicines and Healthcare products Regulatory Agency); the health secretaries for England and Wales; Nadine Dorries, then Minister for Patient Safety Prevention and Mental Health; the then Prime Minister Rishi Sunak – and the National Institute for Health and Care Excellence (NICE).
Tania told me: ‘I’m devastated to hear about Thomas Kingston’s death because it could have been avoided. The story so closely replicates our family’s that I feel angry and let down by so many people.
‘The MHRA has promised to look into this matter, but nearly five years after the needless death of our son another life is cut short that should never have happened.’
annie says
BBC R4 Today programme had a segment on Antidepressants, 07.50, with Danny Kruger, in light of recent developments. Regular guest, Sir Professor Simon Wessely, was absent.,
DK – Beyond Pills
https://www.bbc.co.uk/sounds/play/m0025l1n
Politicians, experts, and patient representatives call for the UK government to reverse the rate of antidepressant prescribing
BMJ 2023; 383 doi: https://doi.org/10.1136/bmj.p2730 (Published 05 December 2023)Cite this as: BMJ 2023;383:p2730
https://www.bmj.com/content/383/bmj.p2730
Beyond Pills APPG
https://beyondpillsappg.org/news/
Lord (David) Alton@DavidAltonHL
Next Wednesday- December 11 – I have secured an oral question in @UKHouseofLords on the failure to adequately warn about the dangerous side effects of some antidepressants on some people. Minister Gillian Merron will reply.
@davidhealyv @markhoro @SyedKamall
How will an International Programme on Educating Doctors work. Does anyone have a plan or will ‘talking shops’ go on forever.
Many professionals talk of ‘helplines’, but who will decide on a ‘final version’ to get off.
Crazily haphazard, at present, as it has always been. I always thought that if someone of a VIP status came along, that all boundaries would be shifted. I wonder if that moment has now come and how will it be wrestled to the ground?
chris says
“kits to ensure a safe night out”
So I read about these kits being handed out at an art fair.
“(Nada) fair in Miami may be surprised to receive an unexpected giveaway: Narcan and safe-sex kits. Part of Casual Safe, an ongoing initiative launched early this year by the Detroit-based arts incubator Buffalo Prescott in partnership with the Detroit Recovery Project, the free kits aim to protect fairgoers and Miami locals alike.:
“Almost everyone has been affected by the opioid crisis, so it becomes crucial to make [overdose reversing treatment] Narcan more readily available, as well as to give people these other kits to ensure a safe night out,”
“In addition to distributing the kits, the team is organising a panel on addiction and the importance of access to harm reduction at Nada on Thursday 5 December at 3pm. Moderated by Osman Can Yerebakan, a writer and curator (and contributor to The Art Newspaper), the conversation will also include Kasztelan and Hannah Meissner, Detroit Recovery Project’s youth programme coordinator.”
So Narcan Naloxone is to reverse opioid overdose. I also read that it can induce rapid on-set opioid withdrawal.
Question – can it therefore induce akathisia as well as what must be a terrible withdrawal or this is not the case?
Harriet Vogt says
Totally agree that it’s unnecessary for patients to add references – as evidence – to the proformas they submit. No need for extra hurdles. By definition any condition that merits a SNOMED or MedDRA code is presumably perceived as medically kosher.
But it was interesting that Mark H’s instincts – ofc he’s both doctor and patient – were to advise his patients to attach the NICE and RCPsych guidance on AD withdrawal to the SNOMED code they submitted to their doctors (how many actually did, nobody knows). This made sense to me – when a condition is so generally accepted that it’s got its own national guidance – it’s like saying, come on doc, surely you know this?
It’s up to individual patients – it’s their proforma. There is always something to be said for not protesting too much – and just being assertive.and assumptive.
annie says
Very fair, Harriet.
The SNOMED Codes is a huge step forward and alerting doctors with your original idea, could be a winner. Regarding additional information added, it depends on which side of the fence you are sat. Should it be a fait accompli to add NICE guidelines, which have been said to be ‘junk’.
‘And this is in great part down to NICE a creation of the Labour Party – who simply do not want to hear that the academic literature on which Guidelines are based is Fake through and through. A series of honourable men have presided over this, award winning journalists won’t go near the issue, Brenda Hale who tackled Boris Johnson doesn’t want to know and doctors… well doctors.’
https://davidhealy.org/the-nice-before-christmas/
Will doctors even read Guidelines attached, they haven’t taken much notice of anything with 8.7 million prescriptions for antidepressants.
Not running before we can walk. Anything given to doctors should be short, sharp and to the point where it will have most impact. The SNOMED Code with patient profile seems eminently sensible.
Isn’t it all about Power for the Patient, and so including Gov Agency Guidelines misses the point?
Harriet Vogt says
Shrewd point, Annie. It is precisely about power to the patient to assert their OWN medical understanding of their OWN experiences of medication. And you’re quite right, the Impact of this act is quite likely to be diluted by giving prescribers the reading homework – they’ve skipped before.
It’s a work habit in my case. Years of needing to support a creative strategy (nothing serious like the life and death business) with real consumer research (not risk managed company fiction).
Significantly, quoting consumers’ own words and feelings is often the clincher in a commercial argument. How can those who don’t know first-hand – dismiss those who do?
What I find frustrating is the extent to which the NHS Patient Safety Strategy is all about embracing patients as ‘partners in their own safety’. And the system is genuinely trying to do this- especially after the harmful event. But, when it comes to psychotropic drug harms, this too rarely seems to be the case – for many reasons we all know. Knowing – makes them even less tolerable.
‘Central to this work has been the development of ideas to enable patients and their
carers to be partners in their own safety as well as in the safety of an organisation. So
while in Don Berwick’s 2013 report into patient safety in the NHS in England, the plea
for “patients and their carers to be present, powerful and involved” is an important call to
action, we must be mindful of the fact that it spoke to a system that for 70 years has
been both paternalistic and hierarchical. One in which patients were seen and treated,
but their voices rarely heard.’
https://www.england.nhs.uk/wp-content/uploads/2021/06/B0435-framework-for-involving-patients-in-patient-safety.pdf
Our Proforma is bang on strategy. Let’s see if we can make it work.
chris says
This is another case I have been thinking about:
https://www.camdennewjournal.co.uk/article/tributes-to-artist-sarah-cunningham-after-tragic-end-to-search
“The New Journal understands from sources close to the investigation that the 31-year-old was seen on CCTV possibly walking into the tunnel southbound towards Camden Town after missing a train.”
If that was the case it is difficult to understand why she would walk into the tunnel in the early hours and not go back to where she was or call a taxi.
chris says
Another interesting case of a recently discovered painting genius
https://www.newyorker.com/magazine/2024/11/18/the-intensely-colorful-work-of-a-painter-obsessed-with-anime
“Fadojutimi has A.D.H.D.”
“Although she appreciated the enforced break from travel and sociability, the confinement eventually induced severe anxiety. ”
Severe anxiety or akathisia from possible ADHD medication?
“All was not calm, however; in the summer of 2021, Fadojutimi experienced a manic episode, and was involuntarily hospitalized. The incident is not easy for her to talk about, and during our conversations she initially approached the subject and then darted away. “They should have just asked me why I was dancing all the time,” she told me at one point, with dark humor. Being institutionalized had been terrifying: “What was shocking to me was how scary it can be to be told that you have got to live with loads of people that are unwell, and you are saying you are not unwell, and they are also saying they are not unwell—but they really are, and you really are.”
Manic episode or medication akathisia again ?
In 2020, even before that first hospitalization, Fadojutimi had been given a diagnosis of bipolar disorder. She had long suspected that she might have the condition, but the news was still painful. “I cried,” she recalled. “I always thought I was, but there were a lot of emotions in hearing a diagnosis.
“Being bipolar, she told me, “makes my life a misery and a dream at the same time.” She remains under the care of a psychiatrist, and is resigned to the necessity of ongoing treatment, while also being skeptical of the efficacy of the approaches she has tried thus far. She spoke bitterly about the institutional structures for mentally ill patients in the U.K. “All the things that are supposed to give us better mental health—they are not there,” she said. “You can’t go outside. You can’t speak to your loved ones whenever you want.”
This is how it goes ADHD diagnosis then medication patient gets worse possible akathisia diagnosed as mania at the time usually treated with AP’s they go for 400mg of quetiapine and a later diagnosis of bi polar.
Does anyone on here think she will improve and recover or will it get worse for her?
She is in a heck of a lot if danger. If anyone on here wants to try and help Millicent Wilner, a senior director at Gagosian London is probably the person to try.